PARP Inhibitors: How They Work and What They Treat
When your cells get damaged, they rely on a system called PARP inhibitors, a class of drugs that block the PARP enzyme involved in DNA repair, especially in cancer cells with BRCA mutations. Also known as poly(ADP-ribose) polymerase inhibitors, these drugs don’t kill cancer directly—they trap cancer cells in a state where they can’t fix their own DNA, leading to their collapse. This approach works best in cancers that already have broken DNA repair systems, like those tied to BRCA1 or BRCA2 gene mutations.
PARP inhibitors are most commonly used for ovarian, breast, prostate, and pancreatic cancers where these mutations are found. They’re not a first-line treatment for everyone, but for people who’ve tried chemotherapy and still have cancer, they can offer a targeted option with fewer side effects than traditional chemo. The key is matching the drug to the tumor’s biology. If your cancer has a BRCA mutation or another defect in homologous recombination repair, PARP inhibitors can be a game-changer. Drugs like olaparib, niraparib, and rucaparib are the main ones used today, each with slightly different profiles for dosing and side effects.
These drugs work because of a concept called synthetic lethality—where two weaknesses together cause cell death, but either one alone doesn’t. Normal cells can still repair DNA using other pathways, but cancer cells with BRCA mutations can’t. So when you block PARP, those cancer cells have no backup. That’s why they’re so effective in specific cases and so useless in others. It’s not magic—it’s precision.
You’ll also find that PARP inhibitors are often used after chemotherapy, not before. They’re not meant to replace chemo entirely, but to extend the time before cancer comes back. Some people stay on them for years, managing cancer like a chronic condition. Side effects like fatigue, nausea, and low blood counts are common, but most people tolerate them better than full-dose chemo. And unlike some treatments, they don’t require hospital visits—you take them as pills at home.
What’s interesting is how PARP inhibitors connect to other treatments. They’re being tested with immunotherapy, radiation, and even newer gene-targeted drugs. Researchers are also looking at whether they can help people without BRCA mutations—those with other DNA repair flaws. The science is still evolving, but the results so far show promise beyond just ovarian and breast cancer.
Below, you’ll find real-world comparisons and guides that help you understand how PARP inhibitors fit into cancer care. You’ll see how they stack up against other treatments, what to expect when you start them, and how to manage side effects. Whether you’re a patient, a caregiver, or just trying to make sense of your options, these posts give you the facts without the fluff.
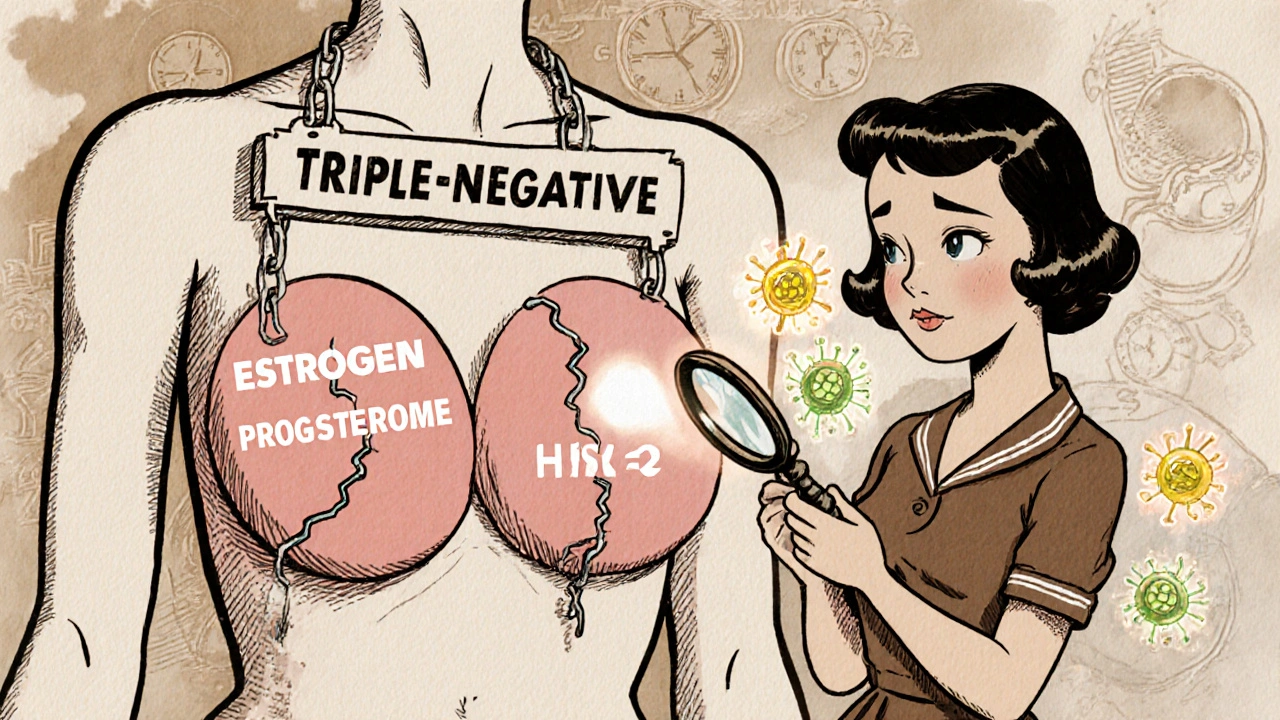
Triple-Negative Breast Cancer: Modern Treatment Strategies and Latest Clinical Trials
- 15 Comments
- Nov, 14 2025
Triple-negative breast cancer (TNBC) is an aggressive subtype with limited treatment options. In 2025, immunotherapy, PARP inhibitors, and antibody-drug conjugates are transforming care. New protocols reduce toxicity while improving outcomes, and personalized vaccines are showing promise in early trials.




