Opioid Withdrawal: Symptoms, Management, and What Helps Most
When someone stops using opioids after regular use, their body goes through opioid withdrawal, a set of physical and mental symptoms that occur as the body adjusts to the absence of opioids. Also known as opioid detox, this process isn’t just uncomfortable—it can feel life-threatening without proper support. It’s not a sign of weakness. It’s biology. Opioids change how your brain handles pain, mood, and stress. When you stop, your nervous system goes into overdrive trying to regain balance.
Common signs include muscle aches, nausea, vomiting, diarrhea, sweating, anxiety, and trouble sleeping. Some people get intense cravings. These symptoms usually start within hours of the last dose and peak around days 2 to 3. For most, they fade within a week, though fatigue and mood swings can linger for weeks. The severity depends on how long and how much someone used, their overall health, and whether they quit cold turkey or taper slowly.
Opioid dependence, a medical condition where the body relies on opioids to function normally isn’t the same as addiction, though the two often overlap. Dependence means your body adapted to the drug. Addiction involves compulsive use despite harm. Many people who become dependent on prescription painkillers never develop addiction—but they still need help getting off the drug safely.
There are effective ways to manage opioid withdrawal symptoms, the physical and emotional reactions that occur when opioids are reduced or stopped. Medications like methadone, buprenorphine, and naltrexone are proven to reduce discomfort and lower relapse risk. Clonidine helps with anxiety and high blood pressure. Over-the-counter remedies like ibuprofen, anti-nausea meds, and hydration can ease minor symptoms. But trying to tough it out alone? That’s where things get dangerous.
Detoxing at home without medical supervision increases the risk of dehydration, seizures, or relapse. Relapse after withdrawal is especially risky—your tolerance drops, so a dose you used to handle can now cause an overdose. That’s why programs that combine medical support, counseling, and long-term planning work best. It’s not just about getting clean. It’s about staying clean.
The posts below cover real situations: how to recognize withdrawal signs before they spiral, what medications help most, why some people relapse even after detox, and how to support someone going through it. You’ll also find advice on managing pain after opioids, avoiding triggers, and what to do if a loved one is struggling. This isn’t theory. These are the tools people actually use to get through it.
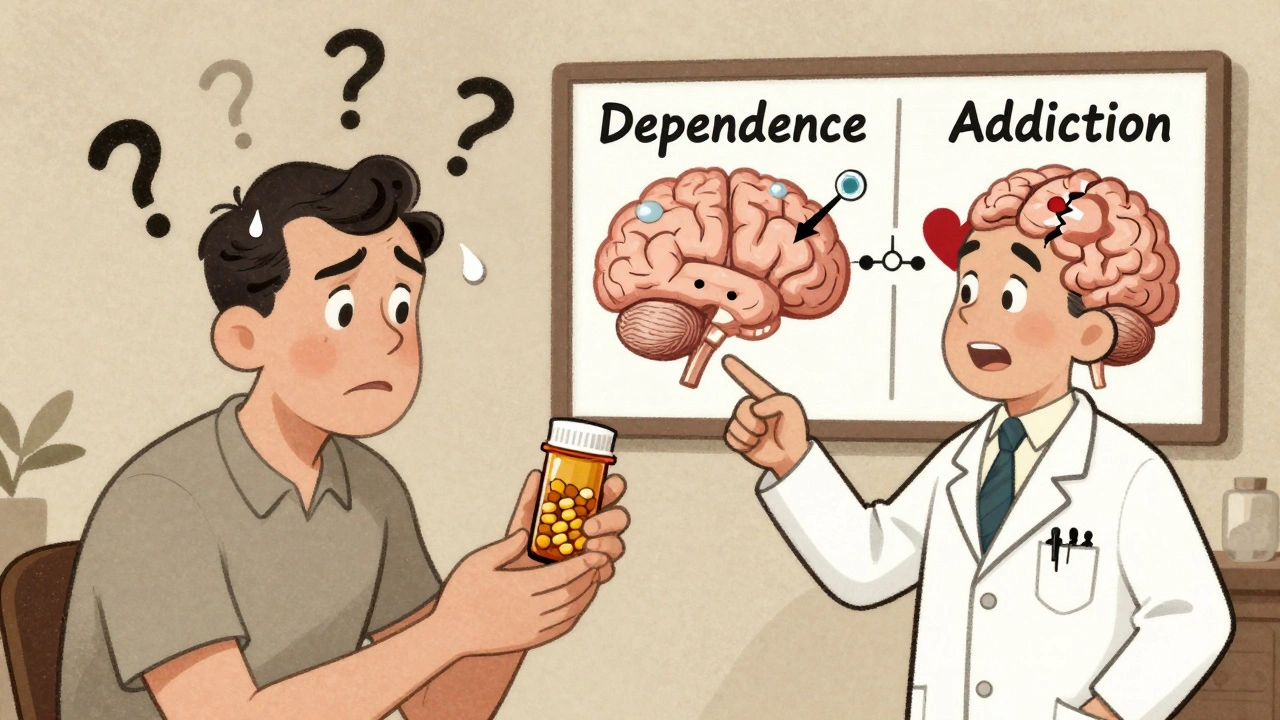
Physical Dependence vs Addiction: Clarifying Opioid Use Disorder
- 13 Comments
- Dec, 1 2025
Understand the critical difference between physical dependence and addiction when using opioids. Learn how withdrawal isn't addiction, why tapering works, and what true Opioid Use Disorder looks like.




