Opioid Side Effects: What You Need to Know Before Using These Pain Medications
When you take opioids, a class of powerful pain-relieving drugs that include oxycodone, hydrocodone, morphine, and fentanyl. Also known as narcotics, they work by binding to receptors in your brain and spinal cord to block pain signals. But they also affect areas that control breathing, mood, and reward — which is why even short-term use can lead to serious side effects.
Common opioid side effects include drowsiness, constipation, nausea, and dizziness. These aren’t just minor annoyances — they can interfere with daily life. For example, constipation from opioids is so common that doctors often prescribe laxatives alongside them. But the bigger risks are less obvious. Opioids slow your breathing, sometimes to dangerous levels. That’s why overdoses happen, especially when people mix them with alcohol or sleep aids. And over time, your body adapts. You need more to get the same relief, and if you stop suddenly, you’ll likely experience opioid withdrawal, a set of physical and emotional symptoms including anxiety, muscle aches, vomiting, and insomnia. This isn’t weakness — it’s biology.
Many people don’t realize that dependence can develop in as little as a week. Even if you’re taking your prescription exactly as directed, your brain starts to rely on the drug to feel normal. That’s why opioid dependence, a physical state where the body needs the drug to avoid withdrawal is different from addiction — though the two often go hand in hand. Addiction involves compulsive use despite harm, while dependence is the body’s physical response. Both require attention. And if you’ve been on opioids for more than a few weeks, quitting cold turkey isn’t safe. Medical supervision helps manage symptoms and reduces the chance of relapse.
Some side effects are rare but deadly. opioid overdose, a medical emergency where breathing stops or slows dangerously can happen if you take too much, if your tolerance drops after a break, or if the drug is mixed with other substances. Naloxone, a life-saving reversal drug, is now available over the counter in many places. Knowing how to use it could save a life — your own or someone else’s.
Below, you’ll find real-world guides on how opioids compare to other pain treatments, what to watch for when switching meds, how to spot signs of misuse, and how to safely reduce or stop use. These aren’t theoretical discussions — they’re based on what patients and doctors are actually dealing with today. Whether you’re taking opioids now, used them in the past, or know someone who is, this collection gives you the facts you need to make smarter, safer choices.
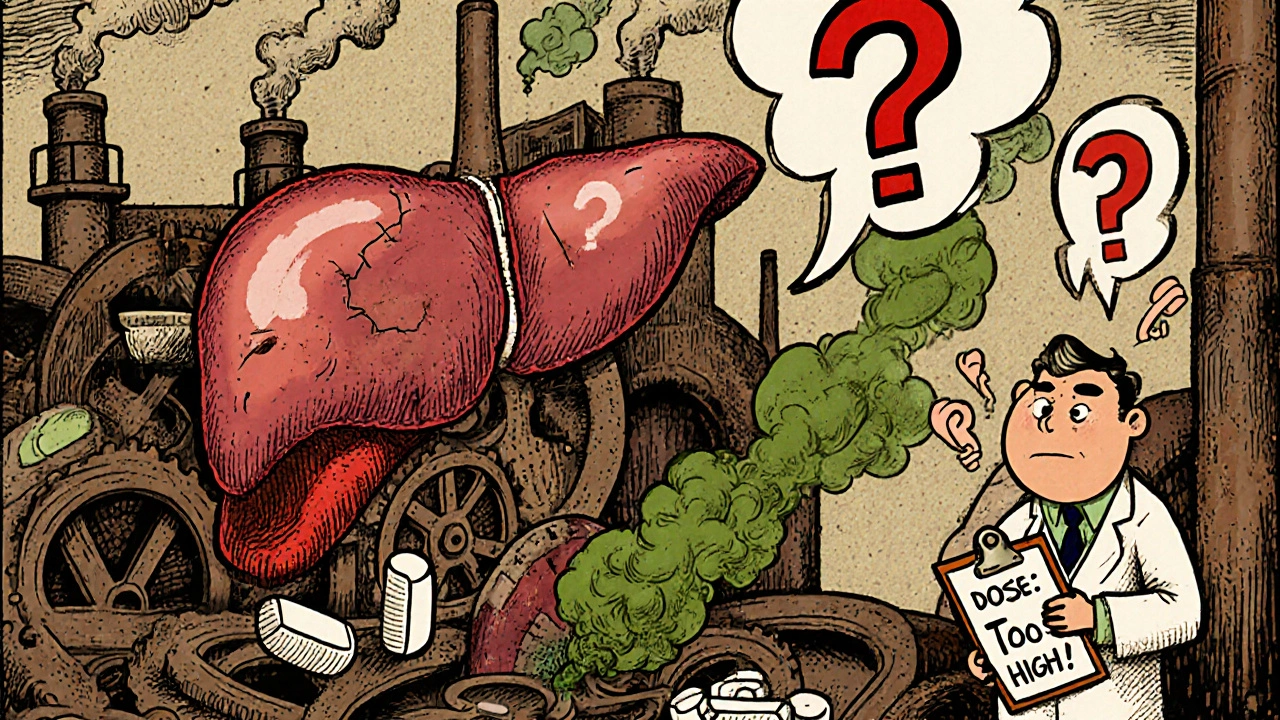
Opioids and Liver Disease: How Impaired Liver Function Changes Drug Safety
- 10 Comments
- Nov, 15 2025
Opioids can become dangerous in liver disease due to impaired metabolism, leading to toxic buildup. Learn how morphine, oxycodone, and other opioids behave in damaged livers-and what safer alternatives exist.




