Opioid Dosing Calculator for Liver Disease
How to Use This Tool
Select your opioid type and liver disease severity to calculate a safe starting dose. Always consult with a healthcare provider before adjusting medications.
Note: This tool provides general guidance but should not replace professional medical advice.
Results
When someone has liver disease, taking opioids isn't just risky-it can be dangerous in ways most people don’t expect. The liver doesn’t just filter toxins; it’s the main factory that breaks down opioids. When it’s damaged, those drugs don’t clear out like they should. They build up. And that buildup doesn’t just make pain relief last longer-it turns into a silent threat. People with cirrhosis, fatty liver, or hepatitis aren’t just getting stronger pain relief. They’re at higher risk of overdose, confusion, breathing problems, and even coma-even at normal doses.
How the Liver Normally Processes Opioids
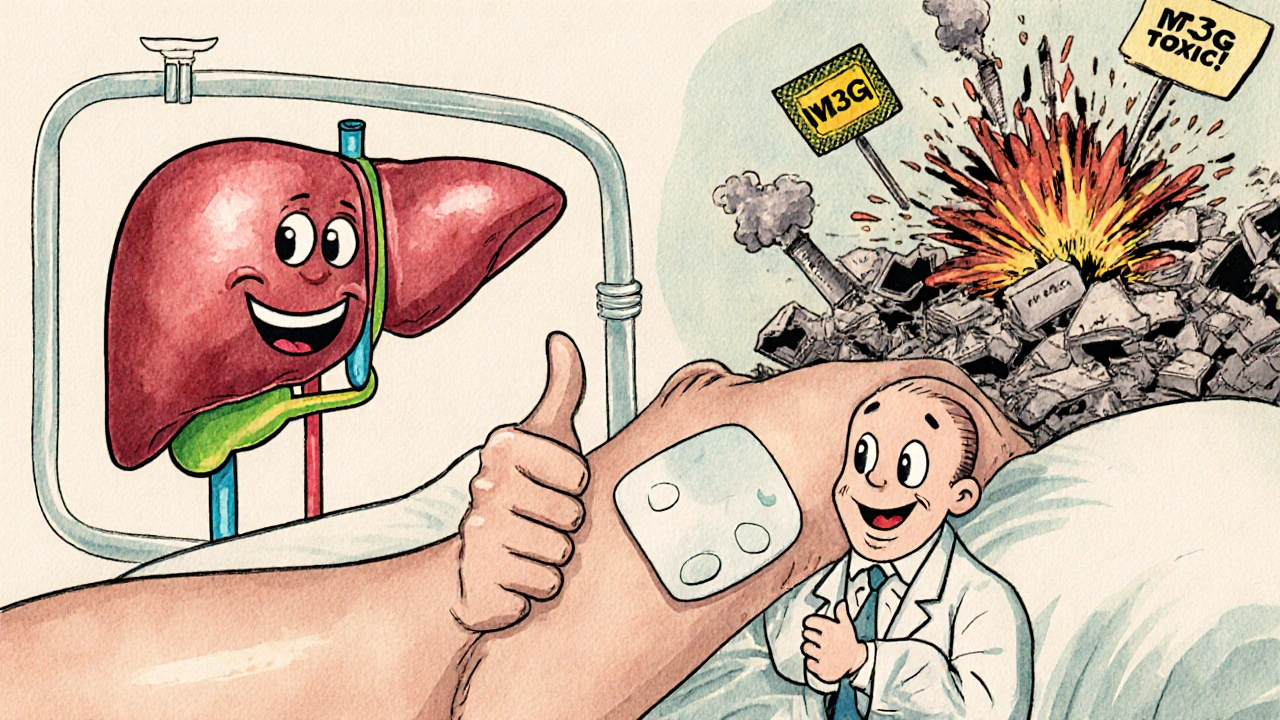
The liver uses two main systems to break down opioids: the cytochrome P450 enzymes and glucuronidation. These are like specialized machines that chop up drugs into smaller pieces so the body can flush them out through urine or bile. Morphine, for example, gets turned into two main metabolites: morphine-6-glucuronide (M6G), which helps with pain relief, and morphine-3-glucuronide (M3G), which does nothing for pain but can cause seizures and nerve irritation. Oxycodone is broken down by CYP3A4 and CYP2D6 enzymes into active forms like oxymorphone. These processes need healthy liver cells and normal blood flow.
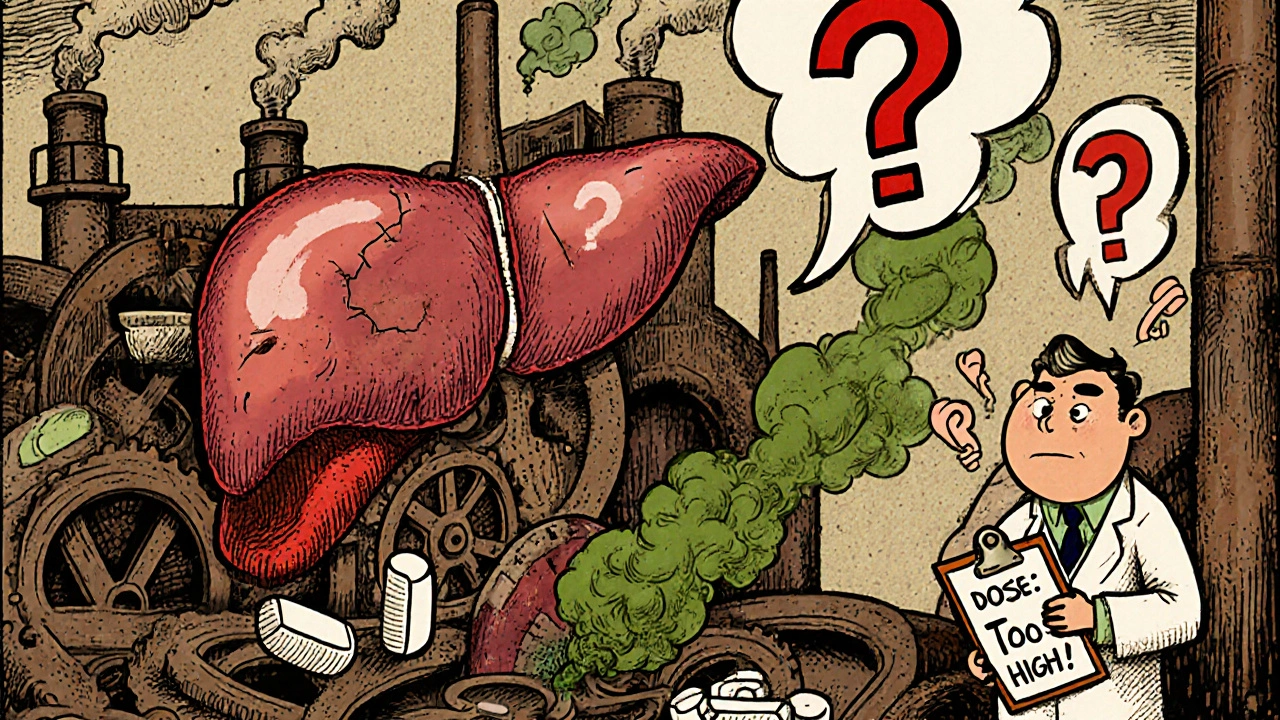
But in a healthy person, this system runs smoothly. In someone with liver disease, the machines start to slow down-or break. The enzymes become less active. Blood flow through the liver drops. And suddenly, a standard dose of morphine or oxycodone doesn’t get cleared. It lingers. That’s when side effects turn from mild drowsiness into life-threatening respiratory depression.
What Happens When the Liver Fails
In advanced liver disease, opioid half-lives can stretch from hours to days. For oxycodone, the normal half-life is about 3.5 hours. In severe liver failure, it can jump to 14 hours on average-and in some cases, stretch as long as 24.4 hours. That means if someone takes a dose every 6 hours, they’re effectively stacking up the drug in their system. By day two, they could have three times the amount of active drug circulating than intended.
Morphine clearance drops by up to 70% in cirrhosis. That’s not a small change. It’s a complete overhaul of how the drug behaves. Even worse, the liver’s ability to make M6G (the good pain-relieving metabolite) declines, while M3G (the toxic one) keeps building up. This creates a double problem: less pain relief and more neurotoxicity. Patients report dizziness, hallucinations, and muscle twitching-not because the dose is too high, but because the wrong metabolites are accumulating.
Alcohol-related liver disease changes things differently. CYP2E1, an enzyme that breaks down alcohol, becomes overactive. That same enzyme also processes some opioids. When it’s overworked, it produces free radicals that damage liver cells further. So in someone with alcoholic cirrhosis, taking opioids doesn’t just accumulate-it may speed up liver damage.
Which Opioids Are Riskiest?
Not all opioids are created equal when the liver is sick. Morphine is one of the worst choices. Because it relies almost entirely on glucuronidation-a pathway that shuts down fast in liver failure-it’s a top concern. Even early-stage disease can make morphine unsafe.
Oxycodone is also risky. In severe liver impairment, peak levels rise by 40%, and the drug sticks around much longer. Guidelines recommend cutting the starting dose to 30%-50% of normal. But many doctors still prescribe standard doses, unaware of how drastically metabolism changes.
Methadone is a gray area. It’s broken down by multiple enzymes, so it doesn’t rely on just one pathway. That sounds good-but there’s no solid dosing guide for liver patients. No clear rules. That makes it unpredictable. Some patients do fine. Others crash.
Transdermal fentanyl and buprenorphine patches may be safer. They bypass the liver’s first-pass metabolism. The drug enters the bloodstream through the skin, not the gut and liver. That means less strain on the liver. For patients with moderate to severe liver disease, these options are often preferred-especially if pain needs to be controlled long-term.
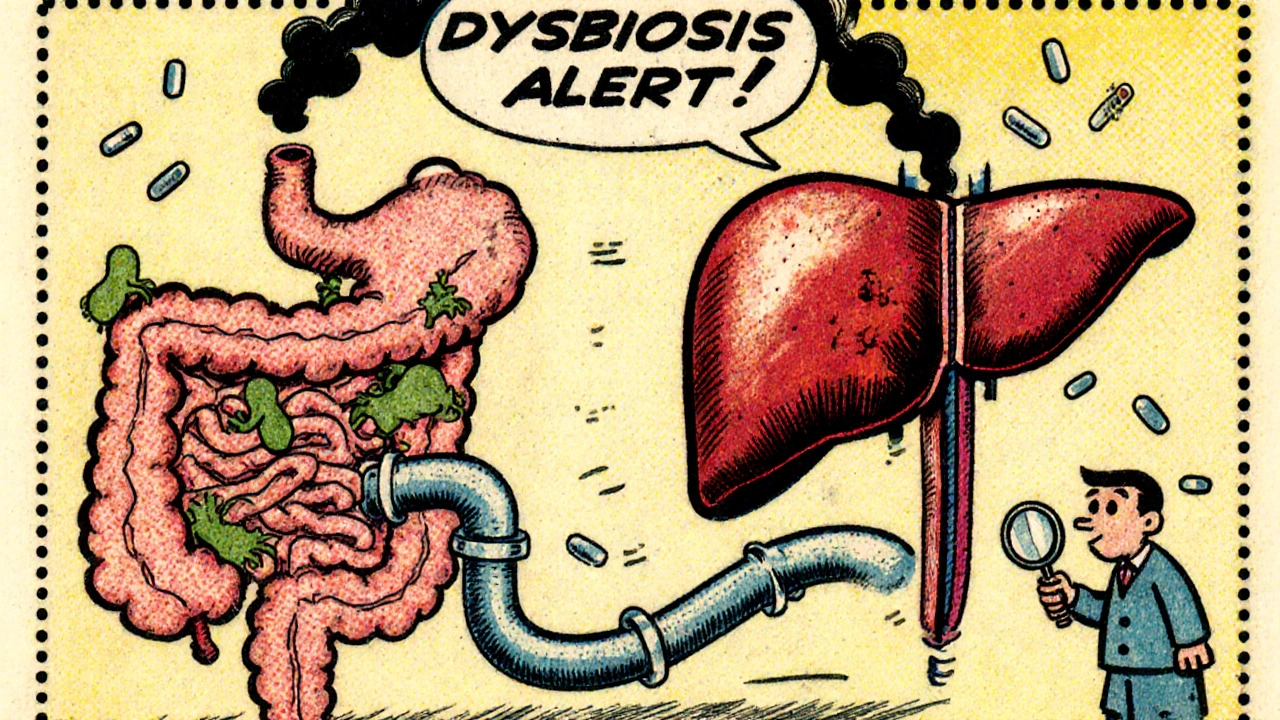
Chronic Use and the Gut-Liver Connection
There’s another hidden risk: opioids don’t just affect the liver-they mess with the gut. Long-term use changes the balance of bacteria in the intestines. This is called dysbiosis. And when gut bacteria get out of whack, they start leaking toxins into the portal vein, which leads straight to the liver.
These toxins trigger inflammation. Inflammation worsens liver damage. In someone with fatty liver disease or hepatitis, that’s a dangerous loop: opioids → gut imbalance → more liver injury → worse opioid metabolism → more toxicity. It’s not just about the drug itself. It’s about how the whole body system breaks down.
Studies show that people with non-alcoholic fatty liver disease (NAFLD) have reduced CYP3A4 activity-even if their liver enzymes look normal. That means even early-stage liver damage can slow opioid breakdown. Many patients don’t know they have NAFLD until it’s advanced. So they’re taking opioids, thinking their liver is fine, while their metabolism is already impaired.
Dosing Adjustments That Actually Work
There’s no one-size-fits-all rule, but here’s what works in practice:
- Morphine: Reduce initial dose by 25%-50% in mild liver disease. In moderate to severe disease, cut the dose by 50%-75% and double the dosing interval (e.g., every 8-12 hours instead of every 4-6).
- Oxycodone: Start at 30%-50% of the normal dose. Avoid extended-release forms. Monitor closely for sedation and breathing changes.
- Methadone: Use only if other options fail. Start low (2-5 mg daily), increase slowly, and check for QT prolongation on ECG.
- Fentanyl patches: Consider for chronic pain. Start with the lowest patch (12 mcg/hour). Avoid in severe liver failure unless closely monitored.
- Buprenorphine: Preferred for chronic pain and opioid use disorder. Less respiratory depression risk. No major dose adjustments needed for mild-moderate disease.
Never assume a patient’s liver is fine just because their blood tests look normal. ALT and AST can be normal even in advanced fibrosis. Use non-invasive tests like FibroScan or APRI scores when available. And always start low, go slow, and watch for subtle signs: confusion, sluggish breathing, unexplained drowsiness.
What We Still Don’t Know
There are big gaps. We don’t have clear dosing guidelines for tramadol, codeine, or hydromorphone in liver disease. We don’t know how much opioid-induced liver injury contributes to progression in NAFLD or hepatitis C. We don’t have large-scale studies on long-term outcomes for patients on opioids with cirrhosis.
Most guidelines are based on small studies or expert opinion. That’s not enough. Doctors need real-world data: how many overdoses happened? How many patients developed hepatic encephalopathy after starting opioids? Until we have that, we’re guessing.
One promising area is pharmacogenomics. Some people naturally have slower CYP2D6 or CYP3A4 activity. Combine that with liver disease, and you’ve got a perfect storm. Testing for these variants could one day guide opioid choices-but it’s not routine yet.
Bottom Line: Safer Pain Management
If you have liver disease and need pain relief, opioids aren’t off the table-but they need a whole new approach. The goal isn’t just to control pain. It’s to avoid poisoning yourself. Start with non-opioid options: acetaminophen (in low doses), NSAIDs (with caution), physical therapy, nerve blocks. If opioids are necessary, choose the safest one for your liver condition, start at a low dose, and never rush to increase it.
Patients and doctors both need to be more aware. A simple question-"Do you have liver disease?"-should trigger a full review of every medication. Opioids aren’t the enemy. But using them the same way in a healthy liver and a damaged one? That’s where the danger lies.
Can I take morphine if I have cirrhosis?
Morphine is generally not recommended in cirrhosis. Its metabolism depends on glucuronidation, which is severely impaired in liver failure. This leads to buildup of toxic metabolites like M3G, increasing the risk of seizures and confusion. Even low doses can be dangerous. Safer alternatives like buprenorphine or transdermal fentanyl are preferred.
Why is oxycodone risky in liver disease?
Oxycodone is broken down by CYP3A4 and CYP2D6 enzymes, both of which slow down in advanced liver disease. This causes the drug to stay in the body longer-half-life can jump from 3.5 hours to over 14 hours. Peak levels rise by 40%, increasing overdose risk. Starting doses should be cut to 30%-50% of normal, and dosing intervals should be extended.
Are fentanyl patches safer than pills for liver patients?
Yes. Fentanyl patches deliver the drug through the skin, bypassing the liver’s first-pass metabolism. This means less strain on a damaged liver and more predictable blood levels. They’re often the preferred choice for chronic pain in patients with moderate to severe liver disease, though close monitoring is still needed.
Can opioids make my liver disease worse?
Yes. Chronic opioid use disrupts gut bacteria, leading to increased toxin release into the liver. This causes inflammation and can speed up fibrosis, especially in fatty liver disease or hepatitis. Opioids don’t directly poison the liver like alcohol-but they create conditions that make existing damage worse.
What’s the safest opioid for someone with liver disease?
Buprenorphine is often the safest option. It’s metabolized by multiple pathways, has a ceiling effect on respiratory depression, and doesn’t rely heavily on liver enzymes. Transdermal fentanyl is also preferred for chronic pain. Both avoid the dangerous metabolite buildup seen with morphine and oxycodone.
Should I avoid opioids completely if I have liver disease?
Not necessarily. Opioids can still be used safely if chosen carefully and dosed properly. The key is avoiding morphine and oxycodone, starting with the lowest possible dose, choosing transdermal or buprenorphine when possible, and monitoring closely for side effects. Non-opioid options should always be tried first.




Philip Rindom
November 17, 2025 AT 18:07Man, I had no idea morphine could turn into a neurotoxin in liver patients. My uncle was on it for back pain and ended up in the ER with confusion - docs just blamed it on "old age." This explains so much. Thanks for laying it out like this.
Jess Redfearn
November 18, 2025 AT 22:11so like… if your liver is messed up, just stop taking pain meds? duh?
Ashley B
November 19, 2025 AT 14:42Of course the pharmaceutical industry doesn’t want you to know this. They’ve been pushing opioids for decades while quietly knowing the liver damage was a side effect they’d rather ignore. The FDA? Complicit. The doctors? Paid off. This isn’t medicine - it’s corporate murder wrapped in a prescription pad. Wake up.
Scott Walker
November 21, 2025 AT 14:14Big respect for this post. 🙌 I’m a nurse in Vancouver and we’ve seen this play out way too often. Buprenorphine patches are a game-changer for our cirrhosis patients. Just wish more docs knew.
Sharon Campbell
November 22, 2025 AT 03:41why do people even need opioids? just do yoga or something. also i think this article is overhyped.
sara styles
November 23, 2025 AT 03:13Let me tell you something - this isn’t just about liver metabolism. It’s about the entire medical-industrial complex using your body as a lab rat. They know that CYP enzymes vary by genetics, they know that NAFLD is silent until it’s too late, and they still pump out standard opioid dosing guidelines like it’s 1999. They don’t care if you’re a 62-year-old with fatty liver and a $200 deductible. They care about the quarterly reports. And the worst part? They’ll tell you to "just take less" - like your liver is a faucet you can turn down. It’s not. It’s a broken engine. And they’re still forcing you to drive it at 80 mph.
Brendan Peterson
November 24, 2025 AT 13:01There’s merit to the pharmacogenomic angle mentioned. I’ve seen patients with CYP2D6 poor metabolizer status on oxycodone - even with normal liver function - develop toxicity. Add liver disease on top? It’s a statistical inevitability. We need genotyping integrated into pain management protocols. It’s not futuristic - it’s overdue.
Rebekah Kryger
November 25, 2025 AT 20:06Transdermal fentanyl is safer? Lol. That’s what they said about the patches during the opioid crisis. Now they’re all over the place in nursing homes. People are dying from fentanyl patches because their skin was sweaty or they took a hot shower. It’s not safer - it’s just less obvious. Same poison, different delivery system.
Victoria Short
November 26, 2025 AT 17:43yeah i guess. i just take tylenol. works fine.
Eric Gregorich
November 26, 2025 AT 18:15Here’s the real question no one’s asking: if opioids are slowly killing the liver through gut dysbiosis, and the liver is the organ that metabolizes them… isn’t that the ultimate paradox? We’re poisoning the very system we rely on to detoxify the poison. It’s like feeding fire with gasoline and calling it a cure. This isn’t just a medical issue - it’s a metaphysical one. We treat symptoms, not systems. We don’t heal bodies; we manage breakdowns. And until we stop seeing the liver as a filter and start seeing it as a living, breathing ecosystem… we’re just rearranging deck chairs on the Titanic.