Opioid Metabolism: How Your Body Processes Pain Medications
When you take an opioid like oxycodone or codeine, your body doesn’t just let it sit there—it breaks it down, transforms it, and gets rid of it. This process is called opioid metabolism, the biochemical process by which the body breaks down opioid drugs to make them easier to eliminate. Also known as drug metabolism, it’s what determines how long the pain relief lasts, how strong the side effects are, and whether a drug will even work for you. Not everyone processes opioids the same way. Some people turn codeine into morphine quickly and feel strong pain relief. Others barely convert it at all—and get little to no benefit. This isn’t about tolerance. It’s about your genes, your liver, and the enzymes that do the work.
The main player in opioid metabolism is the CYP2D6 enzyme, a liver enzyme responsible for activating or breaking down many common opioids. It’s part of a family called cytochrome P450 enzymes. If you’re a fast metabolizer, you turn codeine into morphine faster than normal. That can mean better pain control—or dangerous overdose risk. If you’re a slow metabolizer, you might as well have taken sugar pills. And then there’s CYP3A4, another key enzyme that breaks down drugs like fentanyl and oxycodone. Some medications, like certain antidepressants or antibiotics, can block or boost these enzymes, changing how opioids work in your body. That’s why mixing pills can be risky—even if they’re prescribed by different doctors.
Age, liver disease, and even what you eat can change how opioids are metabolized. A 70-year-old with fatty liver processes drugs slower than a healthy 30-year-old. Grapefruit juice can slow down CYP3A4, making pain meds stick around longer than they should. And if you’ve had a liver transplant or take drugs for hepatitis C, your opioid metabolism could be completely different. This isn’t theoretical. It’s why some people need higher doses, why others get dizzy from a single pill, and why doctors sometimes switch you from one opioid to another—not because the first one stopped working, but because your body stopped processing it right.
Understanding opioid metabolism isn’t just about avoiding side effects. It’s about making sure your pain treatment actually works. The posts below cover real-world cases: how genetic testing helps predict opioid response, why some people get addicted faster due to metabolic quirks, how naloxone interacts with liver enzymes, and what alternatives work better if your body doesn’t handle standard opioids well. You’ll find guides on drug interactions, liver health tips, and comparisons between opioids that behave differently in your system. This isn’t guesswork. It’s science you can use to talk smarter with your doctor and take control of your treatment.
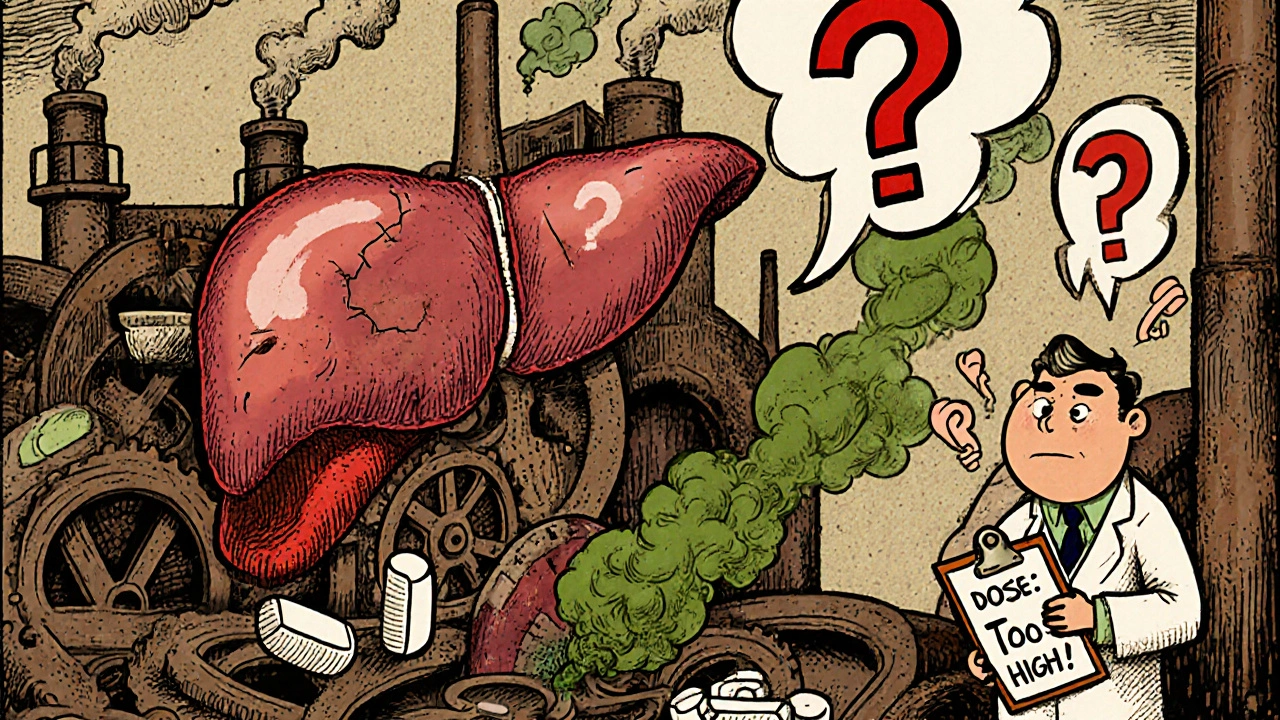
Opioids and Liver Disease: How Impaired Liver Function Changes Drug Safety
- 10 Comments
- Nov, 15 2025
Opioids can become dangerous in liver disease due to impaired metabolism, leading to toxic buildup. Learn how morphine, oxycodone, and other opioids behave in damaged livers-and what safer alternatives exist.




