Opioid Test Sensitivity Calculator
Check if your medication shows up on standard urine tests
Select the opioid you're taking to see if standard urine drug screens will detect it. Based on CDC and ASAM guidelines, this tool shows detection rates and recommended testing strategies.
Why Urine Drug Screens Are Now Standard in Opioid Treatment
When a patient starts long-term opioid therapy for chronic pain, doctors don’t just hand out prescriptions and hope for the best. They need to know if the patient is taking the medication as prescribed - and whether they’re using other drugs that could turn deadly. That’s where urine drug screens come in. These aren’t just random checks; they’re a critical tool to prevent overdose, catch hidden drug use, and protect both patients and providers.
The CDC estimates that in 2021, over 80,000 of the 107,000 drug overdose deaths in the U.S. involved opioids. Many of those deaths happened because patients were mixing prescribed painkillers with illicit substances like fentanyl or benzodiazepines - often without their doctor’s knowledge. Urine testing gives clinicians an objective snapshot of what’s actually in a patient’s system, not just what they say they’re taking.
How Urine Tests Work: Screening vs. Confirmation
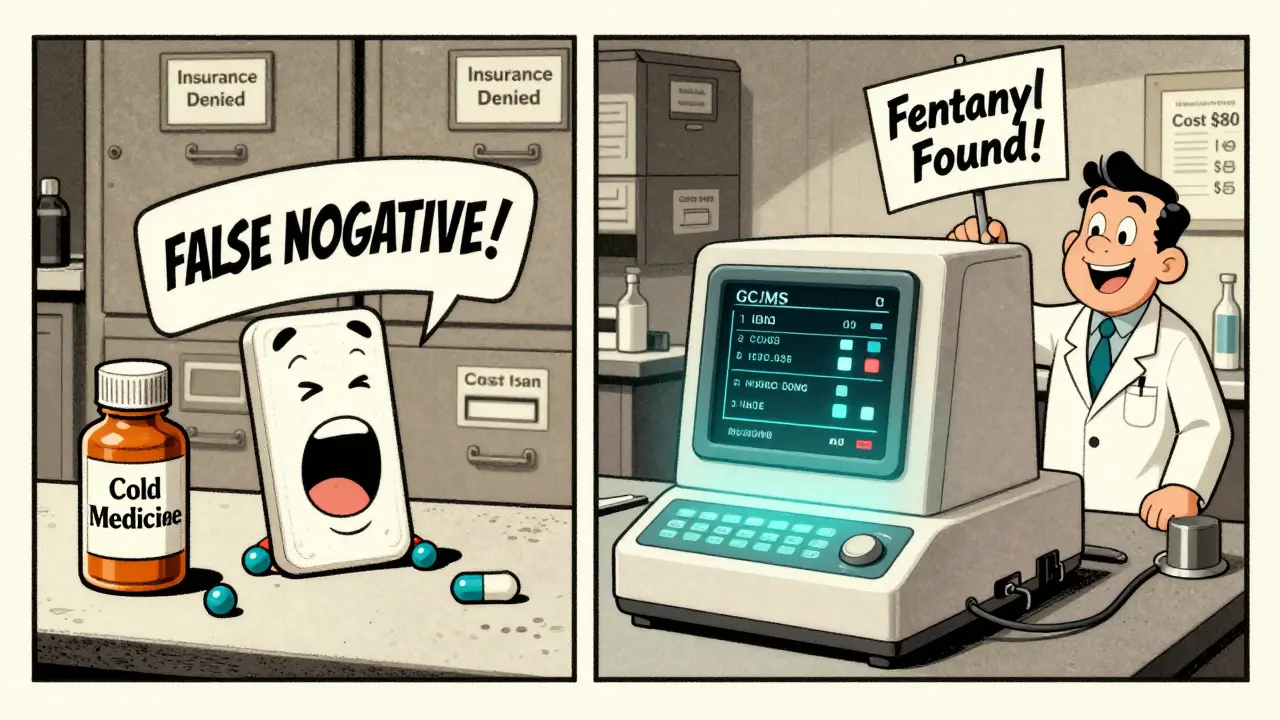
Not all urine tests are created equal. There are two main types: screening tests and confirmation tests. Screening tests, usually done with immunoassays like EMIT, are fast and cheap - around $5 per test. They’re great for catching common drugs like morphine, codeine, or cocaine. But they have a big flaw: up to 30% of results can be false positives. That means a patient might test positive for opioids even if they’ve never taken them, simply because they took a cold medicine or an antibiotic that reacts with the test.
That’s where confirmation testing comes in. Gas Chromatography/Mass Spectrometry (GC/MS) or Liquid Chromatography/Mass Spectrometry (LC-MS) can identify exact drugs and their metabolites. These tests cost between $25 and $100, but they’re accurate. They’re the only way to tell if a patient is taking hydrocodone, for example - because standard immunoassays miss it in over 70% of cases. A 2017 study found that 81 out of 112 patients who tested negative for opiates on a standard screen actually had hydrocodone in their system. Without confirmation, those patients could be wrongly accused of noncompliance.
The Fentanyl Problem: Why Standard Tests Often Fail
Fentanyl is the silent killer in today’s opioid crisis. It’s 50 to 100 times stronger than morphine and often mixed into other drugs without the user’s knowledge. But here’s the catch: most routine urine drug screens don’t detect it. That’s because fentanyl’s chemical structure is too different from morphine-based opioids, which is what most immunoassays are designed to find.
Clinicians are seeing this firsthand. One doctor in a pain clinic in Ohio reported that nearly every patient on a fentanyl patch tested negative on standard panels. Only when they switched to LC-MS testing did they confirm the drug was present. In February 2023, a clinician on a medical forum wrote: “My fentanyl patch patients routinely test negative. We have to send them out for LC-MS - and that’s an extra $80 bill for the patient.”
Thankfully, the FDA approved the first fentanyl-specific immunoassay in 2023. It’s 98.7% sensitive at detecting fentanyl at very low levels. But adoption is still slow. Many labs haven’t upgraded their panels, and insurance often won’t cover the extra cost. So unless you specifically ask for a fentanyl test, it might not be on your screen.
Hydrocodone and Other Hidden Gaps
Hydrocodone is one of the most commonly prescribed opioids in the U.S. - yet it’s notoriously hard to detect with standard tests. A 2022 survey of 1,247 pain specialists found that 68% saw false-negative hydrocodone results at least once a month. Patients get upset. They’re taking their medication, but the test says they’re not. Some even get flagged for “noncompliance” and risk losing their prescription.
Same goes for hydromorphone, oxymorphone, and some synthetic opioids. Even methadone, which is widely used for pain and addiction treatment, can be tricky. While immunoassays for methadone are over 95% accurate, other drugs like buprenorphine can cross-react with tests meant for other substances, leading to false positives and unnecessary disciplinary actions. One 2021 study found that 23% of patients on buprenorphine therapy were wrongly punished because of these test errors.
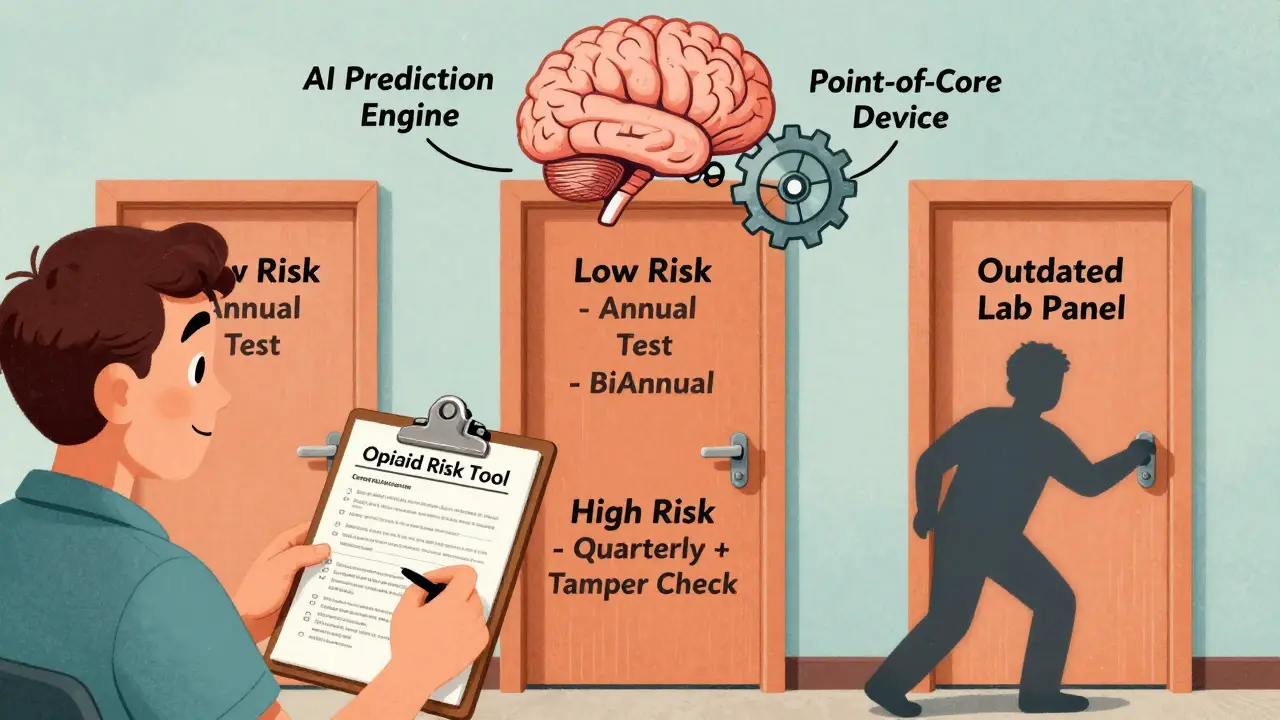
Who Gets Tested - and How Often?
You don’t test everyone the same way. Risk stratification is key. The Opioid Risk Tool (ORT) is a simple five-question questionnaire that helps doctors classify patients as low, moderate, or high risk for misuse. Based on that, testing frequency changes:
- Low-risk patients: One test per year
- Moderate-risk patients: Every six months
- High-risk patients: Every three months, with specimen validity checks
Specimen validity checks are just as important as the drug screen itself. They look for signs of tampering: dilution (too much water), adulteration (bleach or vinegar added), or substitution (someone else’s urine). Medicare and other payers now require these checks on all presumptive tests.
Urine is preferred because it’s noninvasive, easy to collect (30-60 mL), and holds drugs longer than blood. Blood tests are only used in emergencies, like suspected overdose or acute intoxication.
What the Data Shows - and Doesn’t Show
Some doctors assume that if a patient tests positive for their prescribed drug, they’re “adherent.” But that’s misleading. A positive test doesn’t mean they’re taking the right dose. It just means the drug is present. Quantitative testing - measuring exact amounts - is often done, but it’s not clinically useful for judging adherence. A patient could be taking 10 pills a day, or just one - the test won’t tell you which. As Dr. Lynn R. Webster, former president of ASAM, put it: “Quantitative results do not correlate with prescribed doses in clinical practice.”
And here’s another surprise: urine testing doesn’t necessarily reduce illicit drug use. The evidence is weak. But what it does do is change behavior. Patients know they’re being watched. Clinics that use random testing report fewer lost prescriptions and less diversion. One clinic saw a 37% drop in stolen pills after implementing a strict testing protocol.
Market Trends and Real-World Challenges
The urine drug testing market hit $3.1 billion in 2022 and is growing fast - partly because 38 U.S. states now require testing for patients on high-dose opioid therapy. Medicare alone processed nearly 39 million tests in 2022. But the market is dominated by just five labs: Quest Diagnostics, LabCorp, BioReference, Aegis Sciences, and Millennium Health. Together, they control 87% of the business.
That means pricing and test panels vary wildly depending on where you go. A test that costs $20 at one lab might be $85 at another. Insurance doesn’t always cover confirmatory tests, so patients are left paying out of pocket. And many primary care offices still use outdated panels that miss fentanyl, hydrocodone, and synthetic cannabinoids.
What’s Next: AI, Point-of-Care Tests, and Better Guidelines
Change is coming. The CDC is expected to update its opioid guidelines in late 2024, with new emphasis on LC-MS testing for patients on synthetic opioids. The American Medical Association already recommends risk-based testing, not blanket screening.
Point-of-care devices are in development - machines that can give accurate results in under an hour, right in the clinic. Seven are currently under FDA review. And AI tools like the University of Pittsburgh’s Opioid Adherence Prediction Engine are being tested to predict which patients are most likely to misuse opioids based on their behavior, history, and test patterns.
But until those tools are widely available, the best approach is simple: know your test’s limitations. Ask your lab what drugs their panel detects. If you’re on fentanyl or hydrocodone, insist on confirmation testing. And don’t let a false negative or false positive become a reason to stop treatment - or worse, to be punished for something the test got wrong.
What Patients Should Know
If you’re on long-term opioids, understand that urine testing isn’t about distrust - it’s about safety. But you also have rights. Ask:
- What drugs does your panel test for?
- Will you use confirmation testing if the screen is negative but I’m sure I took my meds?
- Are you checking for specimen validity?
- Will you use the Opioid Risk Tool to tailor my testing schedule?
Don’t assume the test is perfect. If your prescribed drug doesn’t show up, push for a second test. Your life might depend on it.




