Morphine and Liver Impairment: Risks, Alternatives, and What You Need to Know
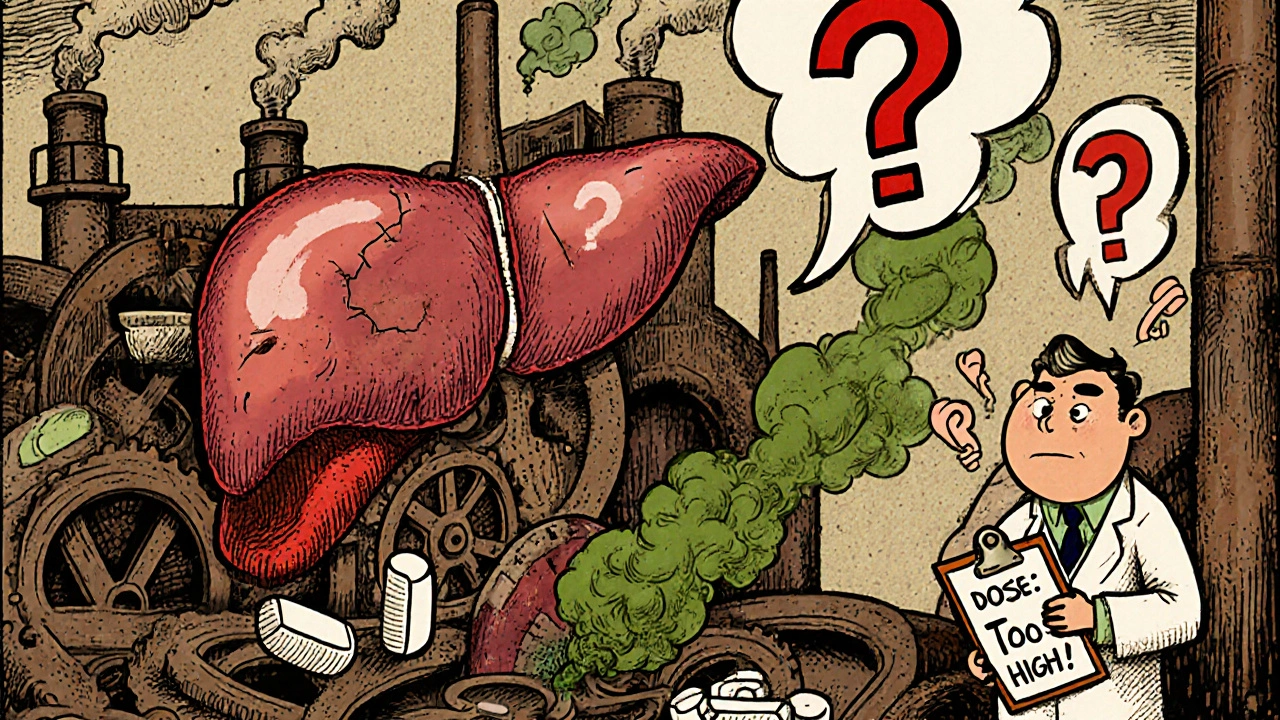
When your liver, the organ responsible for breaking down drugs and toxins in your body. Also known as the body's main filter, it plays a critical role in how medicines like morphine are processed isn't working right, taking morphine, a powerful opioid painkiller used for severe pain, often after surgery or in advanced illness. It's also known as a Schedule II controlled substance, meaning it has high potential for dependence becomes risky. Your liver doesn't just process morphine—it changes it into other compounds, some of which can build up and cause harm if your liver is damaged. People with cirrhosis, hepatitis, or fatty liver disease often need lower doses or completely different pain treatments because their bodies can't clear morphine the way they should.
That buildup doesn't just make you sleepy—it can slow your breathing, lower your blood pressure, or even cause confusion. Studies show that patients with moderate to severe liver impairment can have up to three times the amount of morphine in their blood compared to healthy people, even at the same dose. This isn't theoretical—it's why doctors avoid starting morphine in people with advanced liver disease unless they're closely monitored. Even then, they often switch to drugs like fentanyl or hydromorphone, which are cleared differently and don't rely as heavily on liver enzymes. You might also hear about acetaminophen, a common pain reliever that's safe for most people but can cause serious liver damage if taken in excess. It's often used alongside opioids, but in liver impairment, even this everyday drug can become dangerous. So when you're managing pain and your liver is compromised, it's not just about finding relief—it's about avoiding a bigger problem down the road.
Many people assume that if a painkiller works, it's safe to keep using it. But with liver impairment, that mindset can be deadly. The good news? There are options. Non-opioid treatments like gabapentin or physical therapy can help reduce reliance on morphine. Some patients benefit from nerve blocks or topical patches that deliver pain relief without putting stress on the liver. And if you're already on morphine, your doctor can test your liver enzymes, adjust your dose, or switch you to a safer alternative—without leaving your pain unmanaged. What you'll find in the posts below are real-world guides on how to navigate pain treatment when your body can't process drugs the way it used to. You'll see comparisons of alternatives, warnings about hidden risks, and practical steps to protect your liver while staying comfortable. This isn't just about avoiding side effects—it's about making smarter choices so you don't trade one health problem for another.
Opioids and Liver Disease: How Impaired Liver Function Changes Drug Safety
- 10 Comments
- Nov, 15 2025
Opioids can become dangerous in liver disease due to impaired metabolism, leading to toxic buildup. Learn how morphine, oxycodone, and other opioids behave in damaged livers-and what safer alternatives exist.




