Drug-Induced Hepatitis: Causes, Risks, and What You Can Do
When your liver gets damaged not by alcohol or viruses, but by the very pills you take to feel better, that’s drug-induced hepatitis, a type of liver inflammation triggered by medications, supplements, or toxins. Also known as medication-induced liver injury, it’s more common than most people realize—especially if you’re on multiple drugs or long-term treatments. It doesn’t always show up right away. Sometimes it takes weeks or months of taking a drug before your liver starts sending warning signals.
Many everyday medications can cause this, even ones you think are harmless. Acetaminophen, the active ingredient in Tylenol and countless cold and pain relievers, is the most frequent culprit. Take too much, even just a little over the daily limit, and it can overwhelm your liver’s ability to process it safely. Then there are antibiotics, like amoxicillin-clavulanate or sulfonamides, which some people react to in ways their bodies can’t handle. Even statins, used to lower cholesterol, can cause liver stress in a small number of users. And don’t forget herbal supplements—kava, green tea extract, and some weight-loss products have been linked to serious liver damage.
What makes this tricky is that symptoms often look like the flu: fatigue, nausea, dark urine, yellowing skin or eyes, and right-side abdominal pain. Most people blame it on a virus or stress. But if you’ve started a new medication or changed doses recently, your liver might be reacting. Blood tests—especially liver enzyme levels like ALT and AST—are the only sure way to confirm it. The good news? In most cases, stopping the offending drug early means your liver will heal on its own.
It’s not just about avoiding risky drugs. It’s about understanding how they interact. If you’re taking a painkiller, an antibiotic, and a sleep aid all at once, your liver is juggling more than it can handle. That’s why drug interactions, especially between multiple medications processed by the same liver enzymes, are such a big deal. Your doctor might not catch it unless you tell them everything you’re taking—including vitamins and over-the-counter pills.
People with existing liver conditions, older adults, and those on long-term prescriptions are at higher risk. But anyone can be affected. That’s why checking in with your doctor if you notice unusual tiredness or changes in how you feel is so important. You don’t need to stop all your meds—but you do need to know which ones might be harming your liver, and when to get tested.
Below, you’ll find real-world advice from people who’ve been there—how to recognize the signs before it gets serious, which medications are most likely to cause trouble, and how to talk to your doctor about liver safety without sounding paranoid. These aren’t theoretical tips. They’re based on patient experiences, clinical data, and the kind of practical knowledge you won’t find in a drug label.
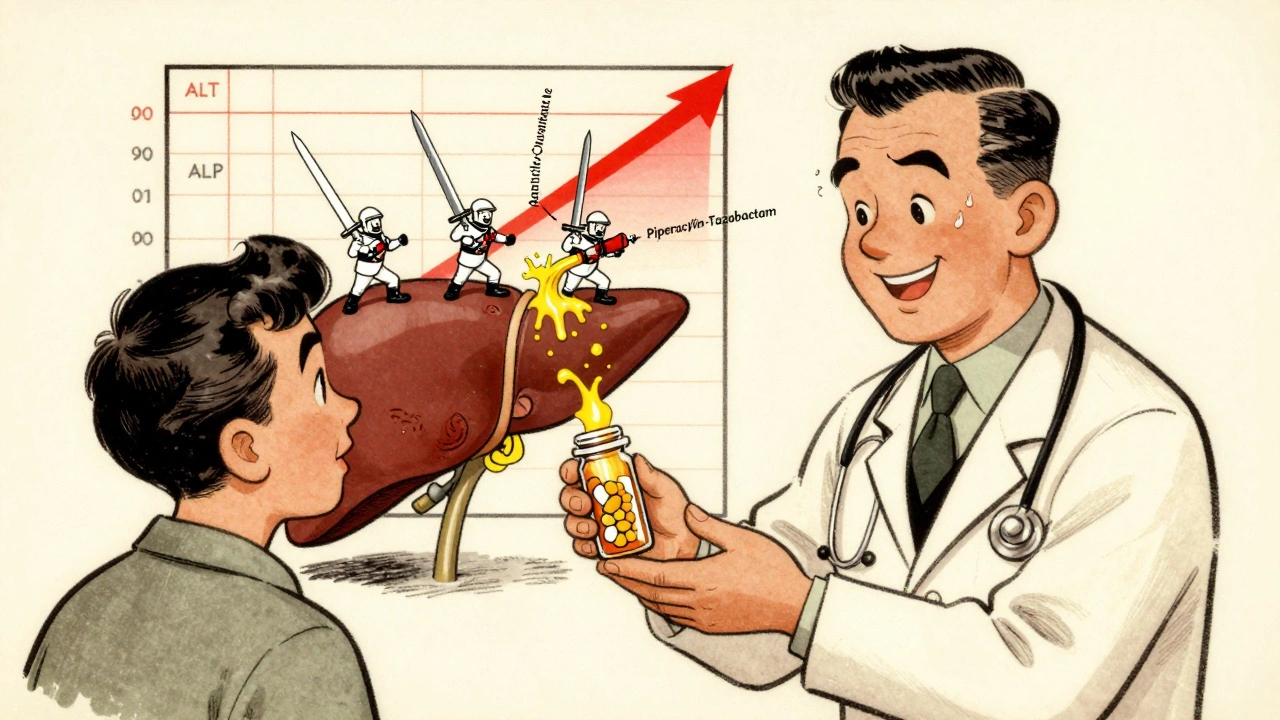
Antibiotic-Related Liver Injury: Understanding Hepatitis and Cholestasis Risks
- 12 Comments
- Dec, 3 2025
Antibiotics can cause liver injury through hepatitis or cholestasis, especially with long-term use. Learn which drugs pose the highest risk, how to spot early signs, and what steps to take for prevention and recovery.