Antibiotic Hepatotoxicity: Signs, Risks, and What You Need to Know
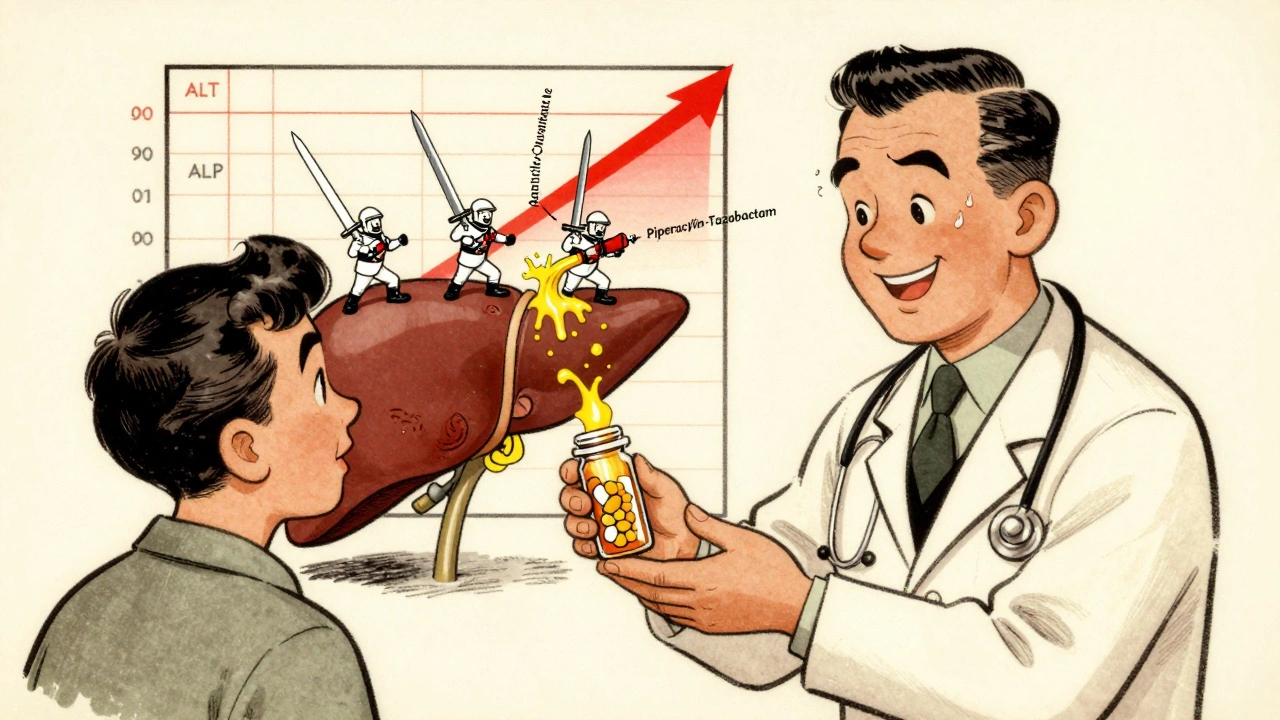
When you take an antibiotic, you expect it to fight infection—not harm your liver. But antibiotic hepatotoxicity, liver damage caused by antibiotics, even those considered safe. Also known as drug-induced liver injury, it’s not rare, and most people don’t realize it’s happening until it’s advanced. This isn’t about rare drugs or overdoses. It’s about everyday prescriptions like amoxicillin-clavulanate, erythromycin, and even tetracycline—medications you’ve probably taken without a second thought.
Some antibiotics are harder on the liver than others. Tetracycline, a broad-spectrum antibiotic once widely used for acne and infections. Also known as Sumycin, it’s rarely first-line today because of its liver risks, especially in people with existing liver issues. Azithromycin, a popular choice for respiratory infections, has been linked to elevated liver enzymes in clinical reports. And amoxicillin-clavulanate, a common combo for sinus and ear infections, causes more cases of liver injury than almost any other antibiotic. These aren’t outliers—they’re the most frequent culprits in real-world cases.
You won’t always feel it coming. No stomachache, no fever. Just fatigue, yellow eyes, dark urine, or unexplained nausea. These are the quiet red flags. If you’ve been on antibiotics for more than a week and start feeling off, don’t brush it off. Liver damage from drugs doesn’t always show up on routine blood tests right away. It builds slowly. And once it’s there, stopping the drug isn’t always enough—you might need monitoring, even hospital care.
It’s not just about the drug. Your age, other meds, alcohol use, and even genetics play a role. Someone on multiple medications—like a statin for cholesterol and a painkiller for back pain—has a higher risk. That’s why medication interactions, how drugs affect each other inside your body. Also known as drug-drug interactions, they’re a silent multiplier of risk. A simple combo like amoxicillin and ibuprofen might seem harmless, but together they can push your liver past its limit.
And here’s the thing: most people who get antibiotic hepatotoxicity didn’t know they were at risk. No one warned them. They followed the prescription exactly. That’s why awareness matters more than ever. You don’t need to avoid antibiotics—you need to know how to use them safely. That means asking your doctor: "Is this the safest option for my liver?" and "What symptoms should I watch for?"
Below, you’ll find real stories and science-backed advice on how antibiotics affect your body beyond just killing bacteria. You’ll learn which drugs are riskiest, how to spot early warning signs, and what to do if you think something’s wrong. No fluff. No guesswork. Just what you need to protect your liver while still getting the treatment you need.
Antibiotic-Related Liver Injury: Understanding Hepatitis and Cholestasis Risks
- 12 Comments
- Dec, 3 2025
Antibiotics can cause liver injury through hepatitis or cholestasis, especially with long-term use. Learn which drugs pose the highest risk, how to spot early signs, and what steps to take for prevention and recovery.




