KDIGO Guidelines: What They Are and How They Shape Kidney Care
When it comes to managing KDIGO guidelines, a set of evidence-based recommendations developed by the Kidney Disease: Improving Global Outcomes organization to standardize kidney disease care worldwide. Also known as Kidney Disease Outcomes Quality Initiative guidelines, they’re the go-to reference for doctors treating chronic kidney disease, dialysis, and kidney-related complications like high blood pressure and anemia. These aren’t just suggestions—they’re the foundation for how hospitals, clinics, and pharmacies decide what treatments work best, when to start them, and how to avoid harm.
KDIGO guidelines don’t just talk about drugs. They cover everything from how to test for early kidney damage using urine albumin and blood creatinine, to when to refer someone for a transplant. They tell you how to manage fluid balance in someone on dialysis, what blood pressure target is safest for a diabetic with kidney disease, and even how to choose between different types of phosphate binders. These rules are updated regularly based on new clinical trials, not opinions. For example, their 2021 update on blood pressure control in chronic kidney disease changed how millions of patients are treated—lower targets aren’t always better, and pushing too hard can do more harm than good.
You’ll also find clear advice on when to use certain medications. For instance, they warn against using NSAIDs in people with reduced kidney function because those drugs can crash kidney function fast. They explain why certain diuretics work better than others in specific cases, and why some blood pressure meds like ACE inhibitors or ARBs are first-line—but only if you monitor potassium and kidney numbers closely. Even something as simple as how often to check lab values is spelled out. This isn’t academic theory. These are the exact rules nurses follow when they call a doctor about a rising creatinine, or when a pharmacist flags a dangerous drug combo.
The guidelines also tackle real-world problems like access to care. They point out that people in low-income countries often don’t get the same tests or meds as those in wealthy ones—and they push for practical, affordable solutions. That’s why you’ll see recommendations for low-cost dialysis regimens, or using generic drugs like furosemide instead of expensive alternatives when the outcome is the same.
What’s in the collection below? Real stories and practical breakdowns of how these rules play out. You’ll find posts on what happens when someone skips dialysis, how to tell if a kidney patient is getting too much fluid, why some meds are dangerous for people with weak kidneys, and how to avoid common mistakes in home care. These aren’t abstract concepts—they’re the daily decisions that keep people out of the ER. Whether you’re a patient, caregiver, or just trying to understand your own labs, the posts here connect the dots between the KDIGO guidelines and what actually happens in real life.
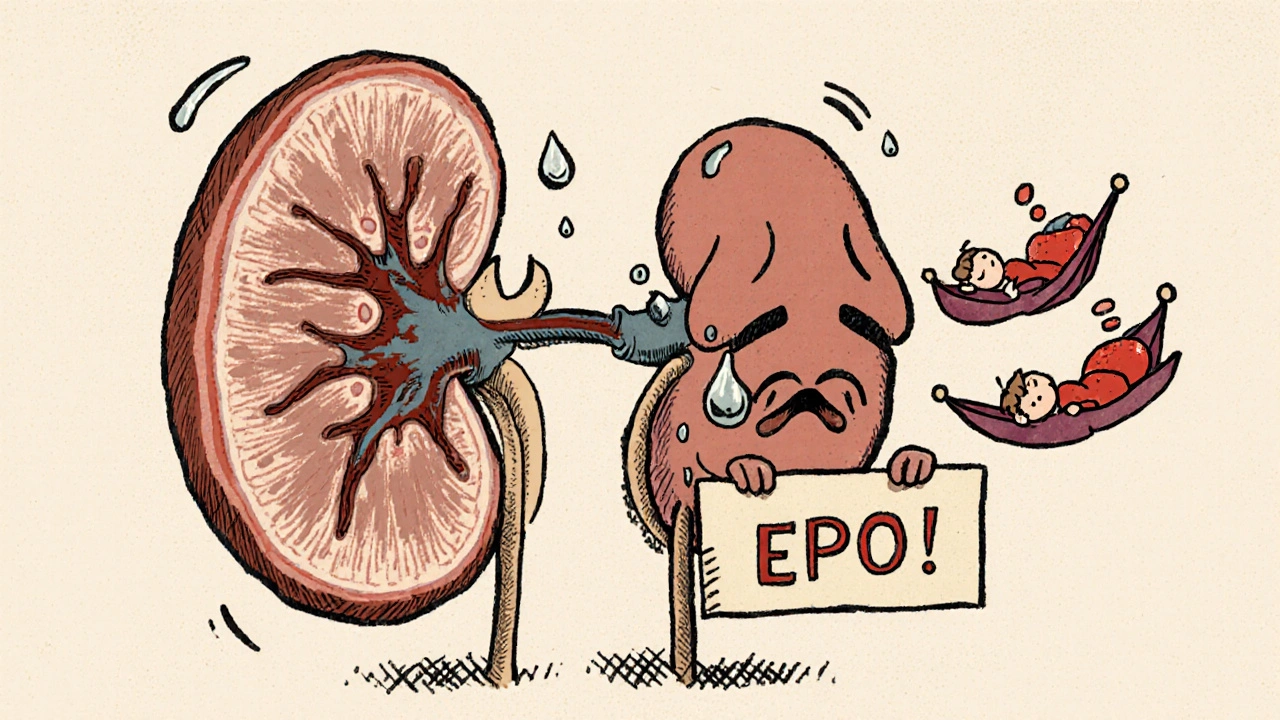
Anemia in Kidney Disease: How Erythropoietin and Iron Therapy Work Together
- 13 Comments
- Nov, 28 2025
Anemia in kidney disease is caused by low erythropoietin and poor iron use. Learn how IV iron and ESA therapy work together to restore energy and reduce risks, based on the latest 2025 KDIGO guidelines.