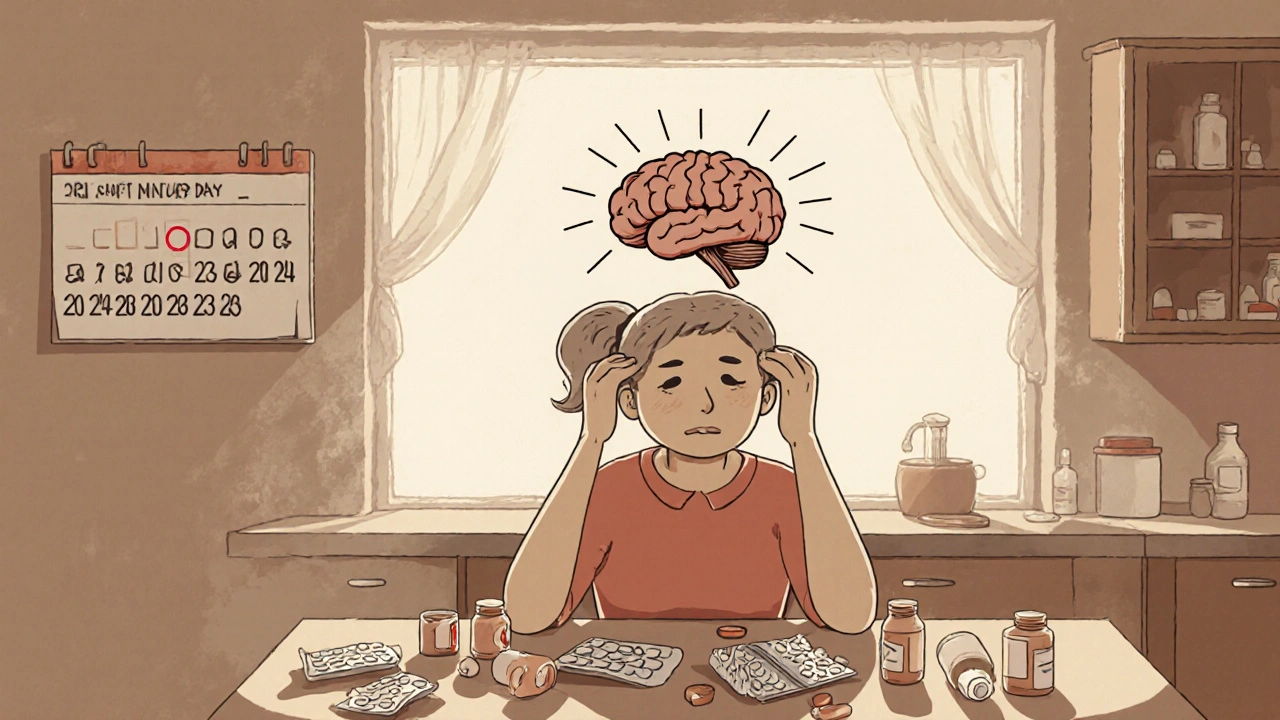
Drug-Induced Headache: Causes, Common Medications, and How to Manage It
When you take a pill to feel better, you don’t expect it to give you a headache—but that’s exactly what happens with drug-induced headache, a type of headache triggered by the use or overuse of medications. Also known as medication overuse headache, this isn’t just a side effect—it’s a cycle that can turn occasional headaches into daily pain. It happens when your body gets used to a drug, and when the effect wears off, your brain reacts with pain. This isn’t rare. Studies show that over 2% of adults worldwide deal with this kind of headache, and it’s one of the most common reasons people end up in neurology clinics.
Many of the drugs we take for pain, allergies, or even mental health can be culprits. opioids, painkillers like codeine or oxycodone are big offenders—especially when used more than 10 days a month. combination pain relievers, like those with caffeine, acetaminophen, and aspirin, are another major cause. Even common OTC meds like ibuprofen or naproxen can trigger this if you’re taking them daily for weeks. And here’s the twist: the very drugs meant to stop your headache end up making it worse over time. This is called a rebound headache, and it’s a sneaky trap because you feel relief right after taking the pill—so you take more, thinking it’s helping.
It’s not just painkillers, either. Hormonal drugs like ethinyl estradiol, found in birth control pills, can trigger headaches in some women. Blood pressure meds like midodrine, used for low blood pressure, and even some antidepressants have been linked to headache changes. The pattern is clear: if you’re taking a drug regularly and your headaches are getting more frequent or more intense, the medication might be the cause.
What makes this tricky is that the symptoms feel real—you’re not imagining it. The pain is often dull, constant, and worse in the morning. It can mimic a tension headache or even a migraine. But unlike a regular headache, it doesn’t respond well to more pills. In fact, the more you take, the worse it gets. Stopping the drug is the only real fix, but that’s easier said than done. Withdrawal can cause a temporary spike in pain, which is why doctors often recommend a supervised taper.
You don’t need to suffer through this alone. The posts below cover real cases and practical steps: how to recognize the signs, which medications are most likely to trigger it, how to safely reduce your use, and what alternatives exist. You’ll find guides on managing headaches caused by hormonal meds, painkillers, and even antibiotics. Whether you’re trying to break free from daily pain relievers or understand why your new blood pressure drug gave you a headache, you’ll find answers here—no fluff, no guesswork, just clear, actionable info.
Medication Overuse Headaches: How to Identify & Find Relief
- 14 Comments
- Oct, 24 2025
Learn how to spot medication overuse headaches, which drugs cause them, and step‑by‑step ways to withdraw and prevent future pain.




