Stopping benzodiazepines cold turkey can be dangerous. For people who’ve been taking them for weeks or months - even if it was prescribed - suddenly quitting can trigger seizures, panic attacks, hallucinations, or worse. The good news? You don’t have to do it alone. With the right plan, most people can safely reduce their dose and break free from dependence without severe withdrawal.
Why Tapering Matters
Benzodiazepines like Xanax, Valium, and Klonopin work fast. They calm anxiety, help you sleep, and stop seizures. But after more than a few weeks, your brain starts to rely on them. When you stop, your nervous system goes into overdrive. That’s withdrawal. And it’s not just feeling jittery. It can mean heart palpitations, intense insomnia, muscle spasms, or even seizures. The 2024 Joint Clinical Practice Guideline, backed by 10 major medical societies, says tapering isn’t optional for long-term users. It’s the standard of care. Abruptly stopping after daily use for over a month raises your risk of severe withdrawal by 20-40%. Tapering cuts that risk dramatically.How Slow Should You Go?
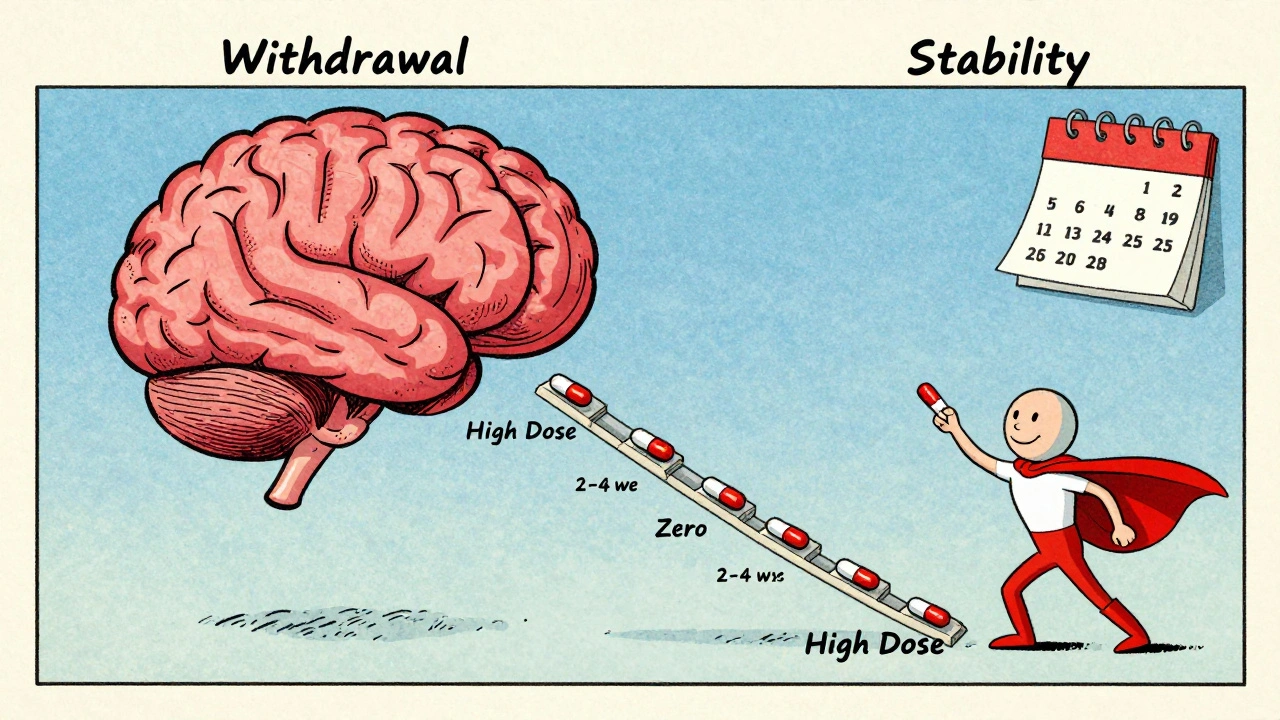
There’s no single timeline that fits everyone. But experts agree: slower is safer. The most widely recommended approach is reducing your daily dose by 5-10% every 2 to 4 weeks. That’s not a guess - it’s based on decades of clinical data showing this pace keeps withdrawal symptoms manageable for most people. Here’s what the Oregon Health Authority recommends based on how long you’ve been taking benzos:- 2-8 weeks of use: taper over at least 2 weeks
- 8 weeks to 6 months: taper over at least 4 weeks
- 6 months to 1 year: taper over at least 8 weeks
- More than a year: taper over 6 to 18 months
Which Benzo Should You Taper From?
Not all benzodiazepines are the same. Their half-lives - how long they stay in your body - make a big difference in how you taper. Short-acting benzos like alprazolam (Xanax) and triazolam (Halcion) leave your system fast. That means withdrawal symptoms can hit hard and quick. If you’re on Xanax, switching to a longer-acting alternative like diazepam (Valium) often makes tapering smoother. Diazepam is the gold standard for substitution. It breaks down slowly and evenly, giving your brain a steadier signal as you reduce. The conversion is simple: 1 mg of alprazolam equals about 20 mg of diazepam. Your doctor will use this to calculate your new starting dose. Triazolam is an exception. Because it doesn’t usually cause physical dependence, some experts say it can be stopped without a taper - but only under medical supervision.Three Main Tapering Methods
There are three proven ways to taper, and your doctor will help you pick the best one for your situation:- Same medication taper: You slowly reduce your current benzo. Best for people on low doses or who’ve already been tapering.
- Switch to a longer-acting benzo: Switch from Xanax or clonazepam to diazepam, then taper the diazepam. This is the most common and safest approach for long-term users.
- Adjunctive medications: Use other drugs to ease symptoms. For example, antidepressants like SSRIs can help with anxiety, melatonin for sleep, or beta-blockers for heart palpitations. These don’t replace the taper - they support it.
Who Should Taper?
Tapering isn’t for everyone - but it’s recommended for many. The guidelines say you should consider it if:- You’ve been taking benzos daily for more than 6 months
- You’re over 65 (benzos increase fall risk and memory problems)
- You have a history of substance use disorder
- You’re taking benzos with opioids or stimulants
- You have PTSD, traumatic brain injury, or cognitive decline
What Happens During the Taper?
Withdrawal symptoms don’t always show up right away. Sometimes they creep in days after a dose reduction. Common signs include:- Increased anxiety or panic
- Insomnia or nightmares
- Tremors or muscle twitching
- Sensory sensitivity (lights, sounds feel overwhelming)
- Dizziness or nausea
- Depersonalization (feeling detached from yourself)
Support Is Key
Tapering isn’t just about pills. It’s about changing how you cope. Many people relapse because they haven’t built new tools for managing stress, sleep, or anxiety. Cognitive behavioral therapy (CBT) is the most effective support. Studies show that when CBT is paired with a medical taper, success rates jump from 42% to 68%. That’s a huge difference. Other supports:- Regular check-ins with your prescriber (every 2-4 weeks)
- One pharmacy, one doctor - to avoid double-dipping
- Time-limited prescriptions (e.g., weekly or biweekly refills)
- Peer support from people who’ve done it before
- Tracking symptoms in a journal or app

When Tapering Isn’t the Answer
Some people need to stay on a low dose long-term. If you’ve tried everything - therapy, other meds, multiple tapers - and still can’t function without benzos, that’s not failure. It’s a medical reality. The goal isn’t to quit at all costs. It’s to use the lowest effective dose for the shortest time. If you’re stable, sleeping, not using alcohol or other drugs, and not falling or getting confused - staying on a tiny dose may be the safest choice.What’s Changing in 2025?
The landscape is shifting fast. In 2024, 28 U.S. states now require a tapering plan for prescriptions longer than 90 days. The FDA updated benzo labels in 2019 to warn against abrupt discontinuation. Now, healthcare systems are responding. New tools are coming. The NIH is funding a mobile app that tracks symptoms in real time and suggests dose adjustments based on your input. It’s being tested now and could be available by 2026. More doctors are being trained. It takes 6-12 months for providers to get comfortable spotting subtle withdrawal signs and adjusting tapers. As demand grows - projected to rise 35% by 2026 - this training will become standard.What to Do Next
If you’re thinking about tapering:- Don’t stop on your own. Talk to your doctor.
- Ask if you can switch to diazepam for a smoother taper.
- Request a written taper schedule - with exact doses and dates.
- Ask about CBT or counseling. It’s not optional - it’s essential.
- Get support. Whether it’s a therapist, peer group, or trusted friend - you don’t have to do this alone.
Can I taper off benzodiazepines on my own?
No. Tapering off benzodiazepines without medical supervision can be dangerous. Withdrawal can cause seizures, psychosis, or severe rebound anxiety. Always work with a doctor who understands tapering protocols. Even if you feel fine, your nervous system may be silently adjusting - and that’s where risks hide.
How long does benzo withdrawal last?
Acute withdrawal symptoms usually peak within 1-4 weeks after your last dose reduction and can last 2-8 weeks. But some people experience protracted withdrawal - lingering symptoms like anxiety, brain fog, or sleep issues - for months. This doesn’t mean you’re addicted. It means your brain is healing. Slower tapers reduce the chance of this happening.
Is diazepam better than Xanax for tapering?
Yes, for most people. Diazepam has a long half-life (up to 100 hours), so it clears slowly and evenly from your system. Xanax (alprazolam) has a short half-life (6-12 hours), which causes sharp drops in blood levels - triggering withdrawal symptoms between doses. Switching to diazepam smooths out those spikes and makes tapering far more tolerable.
Can I use marijuana or alcohol to help with withdrawal?
No. Alcohol and marijuana can worsen withdrawal symptoms and increase the risk of relapse. Alcohol interacts dangerously with benzos and can lower your seizure threshold. Marijuana may temporarily ease anxiety but doesn’t address the root cause - and can lead to new dependencies. Stick to evidence-backed supports like CBT and medical supervision.
What if I feel worse after reducing my dose?
That’s common. Withdrawal symptoms often appear 3-7 days after a dose cut. If they’re mild, wait a few more days - your body may adjust. If they’re severe (panic attacks, tremors, confusion), go back to your last dose. Stay there for another 1-2 weeks, then try a smaller reduction. Patience beats speed every time.
Are there any medications that help with benzo withdrawal?
Yes - but they’re supportive, not replacements. SSRIs like sertraline can help with anxiety. Melatonin improves sleep. Beta-blockers like propranolol can reduce heart palpitations. Gabapentin is sometimes used off-label for nerve-related symptoms. Never use these without your doctor’s guidance. They’re tools to make tapering easier - not shortcuts to avoid it.
How do I know if my taper is working?
Success isn’t measured by how fast you finish. It’s measured by how stable you feel. If your anxiety is manageable, your sleep is improving, you’re not having panic attacks, and you’re not craving your old dose - you’re on the right path. Keep tracking symptoms. If you’re feeling worse over time, your taper may be too fast. Adjust with your doctor.
Can I taper if I’m on multiple benzodiazepines?
Yes - but it’s more complex. Taking more than one benzo increases withdrawal risk. Your doctor will likely switch you to a single, long-acting benzo like diazepam first, then taper that one. Never mix or switch between benzos on your own. This can cause dangerous fluctuations in your system.






Regan Mears
December 9, 2025 AT 23:43I remember when I tried to quit Klonopin cold turkey-big mistake. I thought I was fine, but three days in, I was shaking like a leaf and couldn’t sleep. My doctor switched me to diazepam, and it made all the difference. Slow, steady, and with therapy? I’m 14 months clean now. You don’t have to be perfect-just consistent. And yes, some days suck. But you’re not alone.
David Palmer
December 10, 2025 AT 03:04lol why are we all pretending benzos are evil? I’ve been on 2mg Xanax daily for 8 years. I feel fine. My doctor says I’m stable. Why should I risk my mental health for some guideline that doesn’t even know my life?
Doris Lee
December 11, 2025 AT 03:54Hey David, I hear you. Stability matters more than a number on a chart. But if you ever feel like you want to explore cutting back-even just a little-there’s no shame in trying. You’ve already done the hard part: staying alive and showing up. That’s worth celebrating.
Michaux Hyatt
December 12, 2025 AT 06:16For anyone thinking about switching from Xanax to diazepam: the conversion isn’t exact, but 1mg alprazolam ≈ 10-20mg diazepam is the standard starting point. Always go slow. I’ve seen people drop too fast and end up in the ER. The goal isn’t to suffer-it’s to heal. CBT is the real MVP here. Not magic pills. Just tools.
Frank Nouwens
December 13, 2025 AT 23:31It is worth noting that the pharmacokinetic profile of diazepam, with its active metabolites-desmethyldiazepam, temazepam, and oxazepam-provides a prolonged and attenuated plasma concentration curve, thereby mitigating the abrupt neurochemical fluctuations associated with shorter-acting benzodiazepines. This is not anecdotal; it is evidenced in peer-reviewed pharmacodynamic studies.
Kaitlynn nail
December 15, 2025 AT 00:42So we’re just supposed to trade one addiction for therapy? How profound. The real crisis is that we’ve outsourced emotional regulation to pharmaceuticals. But hey, at least now we can journal our feelings while our brains slowly rewire. Deep.
Stephanie Maillet
December 15, 2025 AT 22:51It’s funny, isn’t it? We’re told to taper because our brains ‘relied’ on benzos… but we never question why they were prescribed in the first place. Society doesn’t teach us how to sit with discomfort. So we medicate. Then we’re told to quit. But we’re never given the tools to live without them. The real withdrawal is from a culture that doesn’t hold space for pain.
Jack Appleby
December 17, 2025 AT 06:25Let’s be clear: anyone who claims marijuana helps with benzo withdrawal is either misinformed or lying. Cannabis doesn’t modulate GABA-A receptors like benzos do-it alters CB1 signaling, which can exacerbate anxiety, paranoia, and cognitive fog during withdrawal. And don’t get me started on gabapentin-off-label use without neurochemical monitoring is a recipe for dependence. This isn’t wellness culture. It’s pharmacology.
Rebecca Dong
December 19, 2025 AT 05:26THEY’RE LYING TO US. The FDA didn’t update labels because of ‘science’-they did it because Big Pharma got caught hiding the addiction rates. And now they’re pushing tapering so we’ll go back for more ‘therapy’ and ‘apps’ and ‘peer coaches’-all while they sell antidepressants and sleep meds. Wake up. This is control. Not care.
Sarah Clifford
December 20, 2025 AT 18:01I tried to taper. Lasted 3 days. Had a panic attack so bad I called 911. Now I’m back on 0.5mg Xanax and I’m not ashamed. My life is better than it was when I was ‘trying to be sober’ and crying in the shower every morning. If you’re not in pain, don’t fix it.