Living with COPD means every medication you take-whether for pain, sleep, or high blood pressure-can either help or hurt your breathing. It’s not just about the lung drugs you’re prescribed. Many common pills you might not think twice about can quietly make your COPD worse, trigger a flare-up, or even land you in the hospital. The good news? You can avoid most of these dangers if you know what to look for.
Why Certain Medications Are Dangerous for COPD
COPD isn’t just a cough or wheeze. It’s a chronic condition where your airways are narrowed, your lungs are damaged, and your body struggles to get enough oxygen. When you take a drug that slows down your breathing or thickens mucus, your lungs don’t have the reserve to compensate. That’s when things go wrong. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) reports that about 15-20% of COPD hospitalizations are linked to medications that shouldn’t have been taken in the first place. That’s preventable. And it’s not just one drug-it’s often the combination of several that creates the danger.Opioids: The Silent Respiratory Suppressors
If you’ve been prescribed an opioid for pain-like oxycodone, morphine, or hydromorphone-you need to talk to your doctor about the risks. These drugs don’t just dull pain. They depress the part of your brain that tells your lungs to breathe. In healthy people, that’s manageable. In someone with COPD, even a small dose can cause breathing to slow to dangerous levels. A 2022 study from the American Thoracic Society found that COPD patients on opioids had a 37% higher risk of respiratory failure than those using non-opioid pain relief. The Centers for Disease Control and Prevention (CDC) recorded over 1,200 COPD-related deaths in the U.S. in 2021 tied to opioid use. That’s not a coincidence. It’s a pattern. And it gets worse when opioids are mixed with other sedatives. Taking oxycodone with a sleep aid like zolpidem (Ambien) or a benzodiazepine like diazepam (Valium) can increase the risk of respiratory arrest by up to 400%, according to a 2022 study in Chest Journal. If you’re on any of these, ask your doctor if there’s a safer alternative for pain or anxiety.Benzodiazepines and Sleep Aids: A Dangerous Duo
Anxiety and trouble sleeping are common in COPD. But reaching for alprazolam (Xanax), lorazepam (Ativan), or even over-the-counter sleep aids like diphenhydramine (Benadryl) can backfire. These drugs calm your nervous system-but they also calm your breathing. A 2021 NIH study found that 28% of COPD patients hospitalized for breathing problems had recently taken prescription sleep aids. That’s nearly one in three. The problem isn’t just the drug itself-it’s how it interacts with your already weakened lungs. Even if you’ve taken these before without issue, COPD gets worse over time. What was once tolerable can become life-threatening. If you struggle with sleep, talk to your doctor about non-drug options: breathing exercises, oxygen therapy at night, or cognitive behavioral therapy for insomnia (CBT-I). These are safer and more effective long-term.Non-Selective Beta-Blockers: Hidden Lung Risks
Many COPD patients also have heart disease. That’s why beta-blockers are often prescribed. But not all beta-blockers are the same. Non-selective beta-blockers like propranolol, nadolol, and timolol block receptors in your lungs as well as your heart. This can cause your airways to tighten, making breathing even harder. A 2022 meta-analysis in Respiratory Medicine showed these drugs increase the risk of a COPD flare-up by 31% compared to safer alternatives. The good news? Cardioselective beta-blockers like metoprolol and bisoprolol are designed to target only the heart. They’re much safer for COPD patients. In fact, some studies show they may even improve survival in COPD patients with heart conditions. If you’re on propranolol for high blood pressure or heart rhythm issues, ask your doctor if switching to metoprolol could help. One COPD patient reported a 15% improvement in lung function within three months after the switch. That’s not magic-it’s science.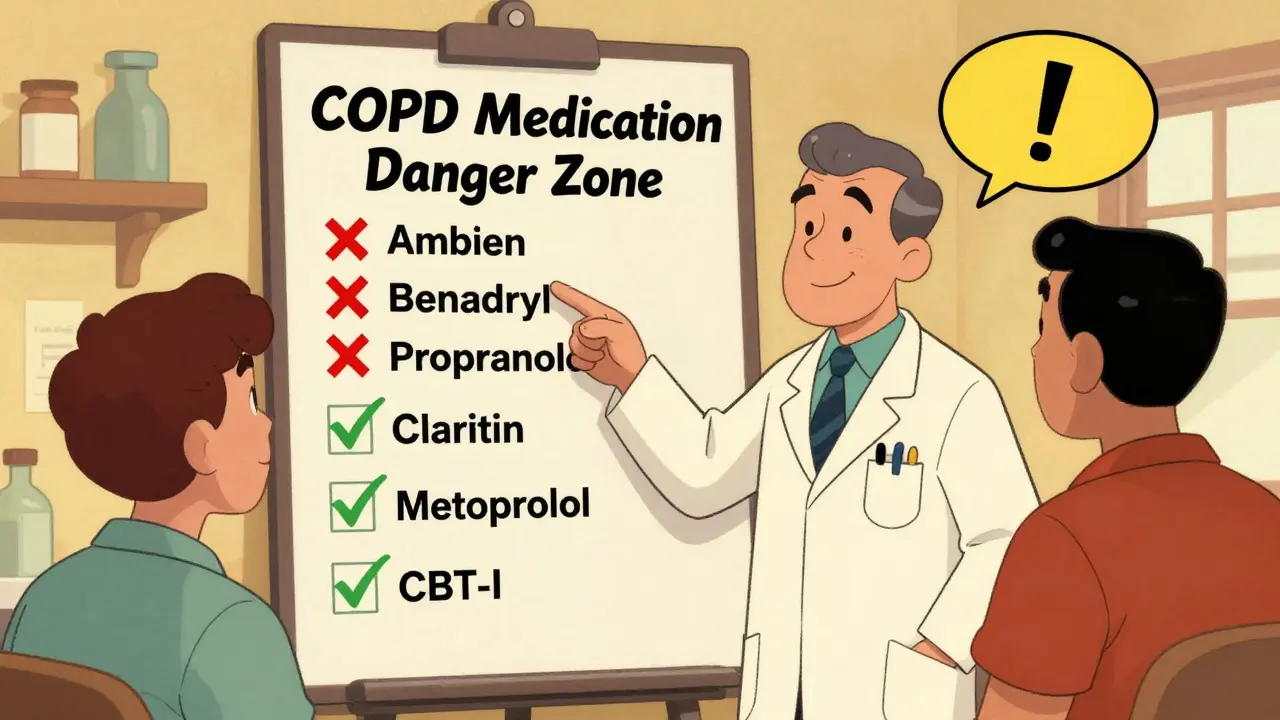
Anticholinergics: Thick Mucus, Worse Breathing
First-generation antihistamines like diphenhydramine (Benadryl), hydroxyzine, and chlorpheniramine are common in cold and allergy meds. But they’re also strong anticholinergics. That means they dry up secretions-including the mucus in your lungs. Sounds helpful? Not for COPD. Thick, sticky mucus is already hard to clear. These drugs make it worse. A 2021 study in Annals of Allergy, Asthma & Immunology found they increase sputum viscosity by 22-35%. That’s enough to trigger a coughing fit or full-blown exacerbation. The same goes for tricyclic antidepressants like amitriptyline. A 2022 study showed 27% of COPD patients on these drugs had worsening breathing, compared to just 9% on SSRIs like sertraline or escitalopram. The American Geriatrics Society’s Beers Criteria (2023) now lists both first-gen antihistamines and TCAs as medications to avoid in older adults with COPD. If you’re taking Benadryl for allergies or sleep, swap it for a non-sedating antihistamine like loratadine (Claritin) or cetirizine (Zyrtec). They don’t thicken mucus.ACE Inhibitors: The Cough That Won’t Quit
ACE inhibitors like lisinopril and enalapril are common for high blood pressure. But about 12-20% of people on them develop a dry, hacking cough. For someone with COPD, that’s a nightmare. It’s not just annoying-it can mimic or worsen your symptoms. The cough hits harder in certain groups: 35% of Asian patients, 25% of African American patients, and 15% of Caucasians. If you’ve started an ACE inhibitor and your cough got worse, it’s likely the drug-not your COPD. The solution? Switch to an angiotensin II receptor blocker (ARB) like losartan or valsartan. A 2022 review in the Journal of Clinical Medicine found ARBs cause 68% fewer cough-related complications than ACE inhibitors. Ask your doctor if switching is right for you.Antibiotics: The Hidden Interaction Trap
Clarithromycin (Biaxin) is often prescribed for chest infections in COPD. But it’s not harmless. It interferes with how your liver breaks down other drugs-especially opioids. A 2021 study in the International Journal of Chronic Obstructive Pulmonary Disease showed clarithromycin can raise opioid blood levels by up to 60%. That’s like doubling your dose without knowing it. Azithromycin is sometimes used long-term to prevent COPD flare-ups. But it can prolong the QT interval on an ECG, raising the risk of dangerous heart rhythms. That’s especially risky if you’re also on other QT-prolonging drugs like certain antidepressants or antifungals. Always tell your doctor what else you’re taking-even if it’s just a supplement. Drug interactions don’t always show up on standard lists.Muscle Relaxers: A Surprising Risk
Cyclobenzaprine (Amrix), methocarbamol, and baclofen are often given for back pain or muscle spasms. But they’re central nervous system depressants. They slow your breathing just like opioids and benzodiazepines. A 2020 study in Mayo Clinic Proceedings found that 22% of COPD patients who started a muscle relaxer needed emergency care for breathing problems within 30 days. That’s a shockingly high number. If you’re prescribed one, ask: Is this absolutely necessary? Can I try physical therapy or heat instead?
What You Can Do Right Now
You don’t have to guess which meds are risky. Here’s what to do:- Do a “brown bag review”: Bring every pill, supplement, and OTC med you take to your next appointment. Let your doctor or pharmacist check them all.
- Ask: “Is this drug on the Beers Criteria list for COPD patients?” If it is, ask for a safer alternative.
- Use the Anticholinergic Cognitive Burden Scale to track how many anticholinergic drugs you’re taking. Even three low-risk ones can add up to a dangerous total.
- Keep a symptom log: Note when you feel worse after starting a new med. That’s a red flag.
- Ask for a pharmacist-led medication review. A 2023 study showed this cuts COPD hospitalizations by 29%.
What’s the Alternative?
You don’t have to live with pain, anxiety, or high blood pressure just because you have COPD. Safer options exist:- Pain: Acetaminophen (Tylenol), physical therapy, nerve blocks, or topical creams.
- Anxiety/Sleep: CBT-I, mindfulness, breathing techniques, or SSRIs instead of benzodiazepines.
- High Blood Pressure: ARBs instead of ACE inhibitors; cardioselective beta-blockers instead of non-selective ones.
- Allergies: Loratadine, fexofenadine, or nasal sprays instead of Benadryl.
- Muscle Spasms: Stretching, heat, massage, or acupuncture.
Final Thought: Your Meds Are Part of Your COPD Management
Your inhalers and oxygen are obvious. But the pills in your medicine cabinet? They’re just as important. Every medication has a cost. For COPD patients, the cost of the wrong drug isn’t just a side effect-it’s a hospital stay, a trip to the ER, or worse. Talk to your doctor. Talk to your pharmacist. Don’t assume something is safe just because it’s prescribed or sold over the counter. Your lungs are already working harder than most. Don’t let a pill make them work harder still.Can I take ibuprofen if I have COPD?
Yes, ibuprofen and other NSAIDs like naproxen are generally safe for COPD patients. They don’t affect breathing or mucus production. But if you have kidney issues or high blood pressure, talk to your doctor first. Long-term use can cause stomach or kidney problems, so use the lowest effective dose for the shortest time.
Is it safe to use CBD oil with COPD?
There’s not enough reliable data yet. While some people report relief from anxiety or pain, inhaling CBD oil through vaping or smoking can irritate your lungs and worsen COPD symptoms. If you want to try CBD, use oral tinctures or capsules-not vaporizers. Always tell your doctor before starting.
What should I do if I accidentally took a dangerous medication?
If you took one of these medications and notice new or worsening shortness of breath, drowsiness, confusion, or slow breathing, seek medical help immediately. Don’t wait. Call your doctor or go to the nearest emergency room. Bring the medication bottle with you. Early intervention can prevent a full respiratory crisis.
Can I stop these medications on my own?
No. Stopping some of these drugs suddenly-especially beta-blockers, benzodiazepines, or opioids-can cause serious withdrawal symptoms or rebound effects. Always work with your doctor to safely taper off or switch medications. Never stop without professional guidance.
Are there any medications that are actually good for COPD patients?
Yes. Inhaled bronchodilators (like salmeterol or tiotropium), inhaled corticosteroids (when needed), and pulmonary rehab are the foundation. Cardioselective beta-blockers, ARBs for blood pressure, and SSRIs for depression are also often safe and beneficial. The key is matching the right drug to your full health picture-not just your lungs.
How often should I review my medications?
At least twice a year. But if you’ve recently been hospitalized, started a new drug, or noticed new symptoms, do it sooner. COPD changes over time, and so should your meds. A pharmacist-led review every 6 months can cut your risk of hospitalization by nearly a third.






siddharth tiwari
December 23, 2025 AT 01:13Diana Alime
December 23, 2025 AT 10:56Adarsh Dubey
December 25, 2025 AT 06:17Bartholomew Henry Allen
December 25, 2025 AT 14:43Jeffrey Frye
December 27, 2025 AT 07:17Andrea Di Candia
December 27, 2025 AT 08:34Usha Sundar
December 27, 2025 AT 12:38Wilton Holliday
December 28, 2025 AT 02:53Joseph Manuel
December 29, 2025 AT 12:47