Anemia in Kidney Disease: Causes, Symptoms, and What You Can Do
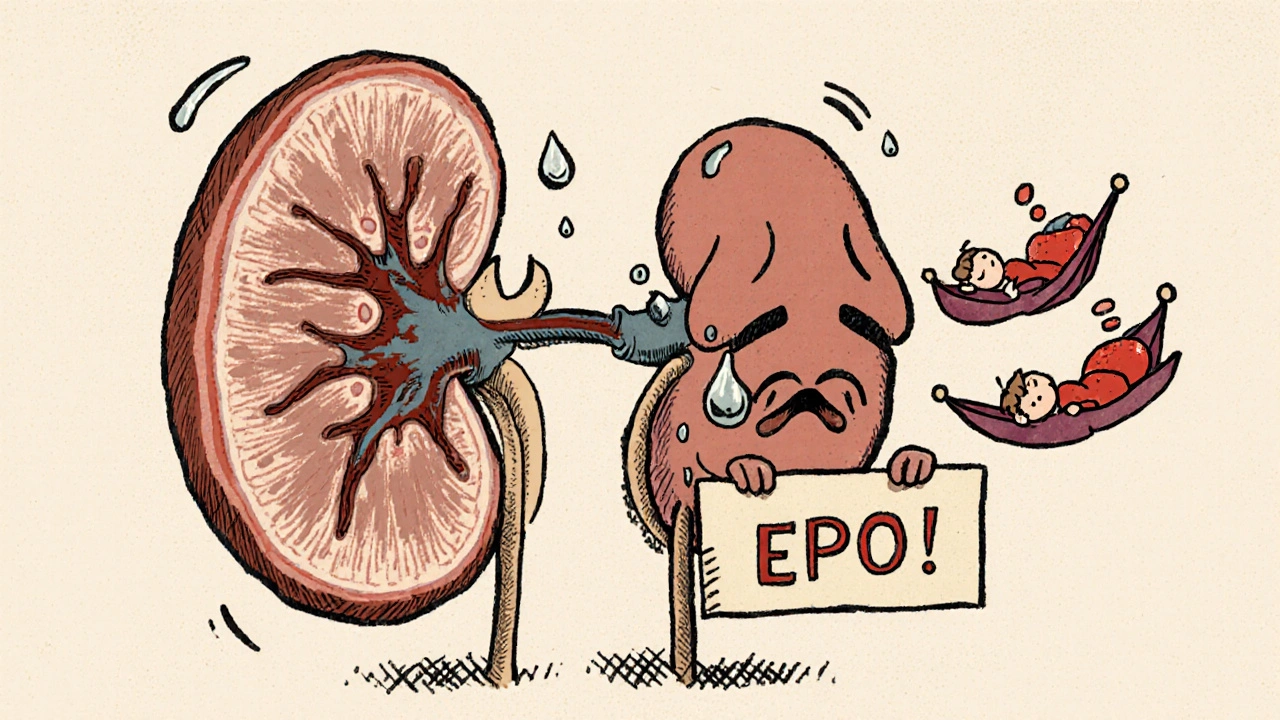
When your kidneys aren’t working right, they stop making enough erythropoietin, a hormone that tells your bone marrow to make red blood cells. Also known as EPO, this hormone is key to keeping your blood oxygenated. Without it, you get tired, dizzy, and short of breath—not because you’re lazy, but because your body literally can’t carry enough oxygen. This is anemia in kidney disease, a condition that affects up to 90% of people with advanced kidney failure. It’s not just low iron—it’s a breakdown in communication between your kidneys and your blood.
Most people think anemia means they just need more iron, but that’s only part of the story. In kidney disease, your body often has plenty of iron stored, but it can’t use it because the kidneys aren’t signaling properly. Even if you take iron pills, your red blood cell count might not budge. That’s why treatments like erythropoiesis-stimulating agents, drugs that mimic the hormone your kidneys should be making are used. But they’re not magic. They work best when paired with proper iron levels, vitamin B12, and folic acid. And if you’re on dialysis, you’re even more likely to lose iron through blood loss during treatments.
Left untreated, this kind of anemia doesn’t just make you tired. It forces your heart to work harder, raises your risk of heart failure, and can speed up kidney damage. Many patients don’t even realize they have it until they’re exhausted all the time or their doctor runs a simple blood test. The good news? It’s usually fixable. The trick is catching it early and treating the root cause—not just the symptom.
Below, you’ll find real, practical posts that break down how anemia in kidney disease works, what meds help (and which ones don’t), how to tell if you’re low on iron versus something else, and what lifestyle changes actually make a difference. No fluff. No guesswork. Just what works.
Anemia in Kidney Disease: How Erythropoietin and Iron Therapy Work Together
- 13 Comments
- Nov, 28 2025
Anemia in kidney disease is caused by low erythropoietin and poor iron use. Learn how IV iron and ESA therapy work together to restore energy and reduce risks, based on the latest 2025 KDIGO guidelines.




