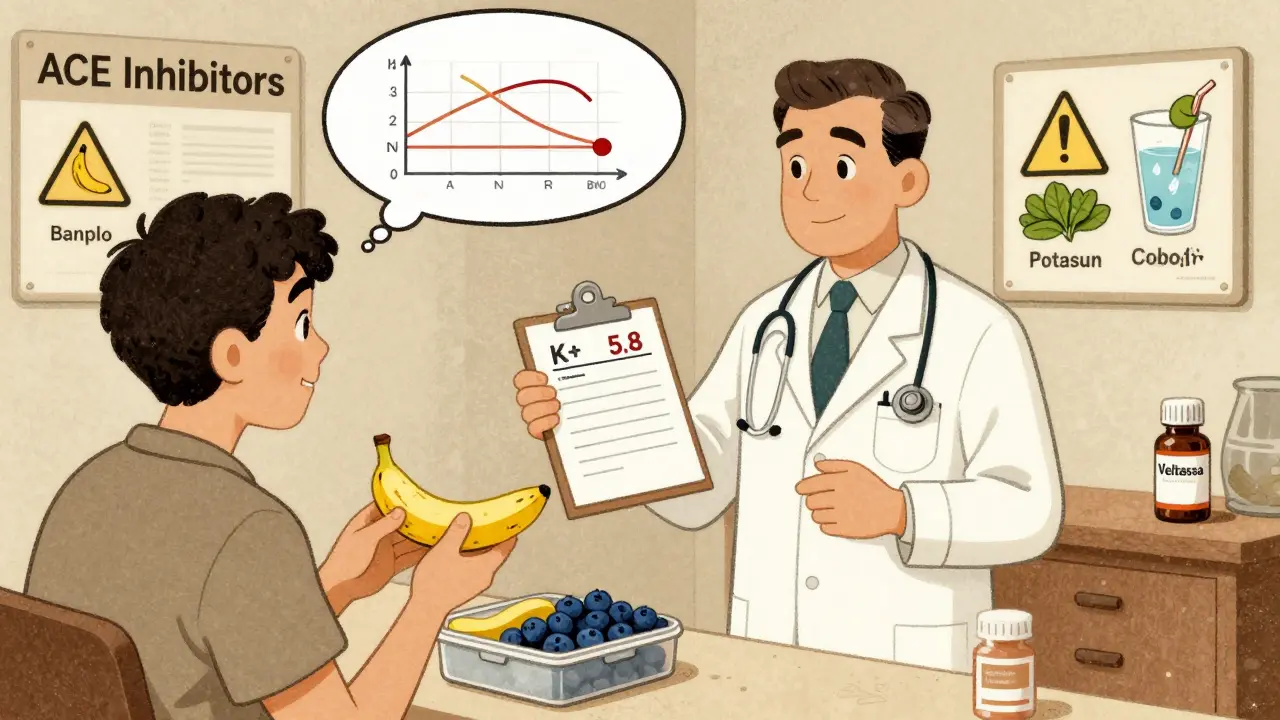
If you're taking blood pressure medication and trying to eat healthier, you might be confused about potassium. Some doctors tell you to eat more bananas and spinach. Others warn you to avoid them. The truth? It depends on what meds you're on. Get it wrong, and you could end up in the hospital. Get it right, and you might lower your blood pressure without adding another pill.
Why Potassium Matters for Blood Pressure
Potassium isn’t just another mineral. It’s a key player in keeping your heart and blood vessels healthy. When you eat enough potassium, your body naturally pushes out extra sodium. That reduces the pressure on your artery walls. Studies show that getting 3,500 to 5,000 mg of potassium daily can drop systolic blood pressure by over 5 mm Hg - that’s about the same as a low-dose pill.The effect is strongest in people who eat a lot of salt. If your diet is heavy on processed food, canned soups, or frozen meals, boosting potassium can make a real difference. Research from the American Heart Association confirms that potassium helps relax blood vessels and reduces fluid retention - without triggering the stress hormones that other drugs might.
But here’s the catch: potassium only helps if your kidneys can handle it. If they’re not working well, too much potassium builds up in your blood. And that’s dangerous.
Which Blood Pressure Meds Raise Potassium Risk?
Not all blood pressure medications affect potassium the same way. Three major classes are known to increase the risk of high potassium levels - a condition called hyperkalemia:- ACE inhibitors - like lisinopril, enalapril, ramipril
- ARBs - like losartan, valsartan, irbesartan
- Potassium-sparing diuretics - like spironolactone, eplerenone
These drugs work by blocking the renin-angiotensin system - a hormone pathway that controls blood pressure. But they also reduce how much potassium your kidneys flush out. That’s good for lowering pressure, but risky if you’re already eating a lot of potassium-rich foods.
Studies show that around 40% of people on high blood pressure meds are prescribed one of these three types. And about 11% of older adults on ACE inhibitors or ARBs develop high potassium when they start eating more fruits, veggies, or salt substitutes. That’s why your doctor should check your potassium levels before and after you make big dietary changes.
High-Potassium Foods: What’s Safe and What’s Risky
You don’t need to avoid all high-potassium foods. But you do need to know which ones pack the biggest punch - and how much you’re eating.Here are common high-potassium foods and how much potassium they contain per typical serving:
- 1 medium banana - 422 mg
- 1 medium sweet potato - 542 mg
- 1 cup cooked spinach - 839 mg
- 1 avocado - 975 mg
- 1 cup cooked lentils - 731 mg
- 3 oz salmon - 534 mg
- 1 cup coconut water - 600 mg
- 1/4 teaspoon potassium salt substitute - 250-700 mg
Notice anything? You can hit over 1,000 mg of potassium in just one meal. That’s nearly a third of your daily goal - and if you’re on a potassium-retaining drug, it’s easy to go overboard.
Some people think they’re being smart by switching to salt substitutes. But those often contain potassium chloride. If you’re on an ACE inhibitor, that’s like adding a potassium pill with every sprinkle. A 2020 study found that using these substitutes raised potassium levels by 0.3 to 0.5 mmol/L on average - enough to push someone near the danger zone.

The Real Danger: Hyperkalemia
High potassium doesn’t always cause symptoms. That’s why it’s so sneaky. But when levels climb above 5.0 mmol/L, you’re in danger. At 6.0 mmol/L or higher, your heart can start beating irregularly - even stopping.Symptoms of hyperkalemia include:
- Muscle weakness or cramps
- Tingling or numbness in hands or feet
- Palpitations or skipped heartbeats
- Feeling unusually tired
- Nausea or vomiting
One survey of 872 people with high blood pressure found that 19% had experienced these symptoms after increasing potassium intake without medical advice. Seven percent ended up in the ER.
And it’s not just about food. People with kidney disease are at much higher risk. If your eGFR (a measure of kidney function) is below 60, you’re 28% more likely to develop hyperkalemia when on ACE inhibitors or ARBs. That’s why doctors often avoid these drugs in advanced kidney disease - unless they’re closely monitored.
What You Can Do: A Practical Guide
You don’t have to give up healthy foods. You just need to be smart.Step 1: Know your meds
Check your prescription bottle. If it says lisinopril, losartan, spironolactone, or eplerenone - you’re on a potassium-retaining drug. Don’t assume it’s safe to eat more bananas just because you heard they’re good for you.
Step 2: Get tested
Ask your doctor for a basic blood test to check your serum potassium. Normal range is 3.5 to 5.0 mmol/L. If you’re at 4.8 or higher, you’re already close to the edge. Don’t wait for symptoms.
Step 3: Track your intake
Use a free app like Cronometer or the National Kidney Foundation’s “Potassium Counts” app. Log your meals for a week. You might be shocked to see how fast your potassium adds up. One avocado and a cup of spinach? That’s nearly 1,800 mg - already 40% of your daily limit if you’re on a restricted diet.
Step 4: Adjust wisely
Instead of cutting out all high-potassium foods, swap some out:
- Swap banana for blueberries (1 cup = 114 mg potassium)
- Swap sweet potato for white potato (peeled, boiled - 540 mg vs. 420 mg)
- Swap spinach for lettuce (1 cup cooked spinach = 839 mg; 1 cup iceberg = 18 mg)
- Avoid potassium salt substitutes unless your doctor says it’s safe
A Reddit user on r/hypertension shared that switching from 3 bananas a day to blueberries and apples brought their potassium down from 5.4 to 4.8 mmol/L - without changing their meds.
When to Talk to Your Doctor
Don’t wait until you feel sick. Schedule a conversation if:- You’ve recently started a new blood pressure med
- You’ve increased your fruit, veggie, or legume intake
- You’re using salt substitutes
- You’ve been told you have kidney issues
- You’re over 65 - older adults are more vulnerable
Your doctor should check your potassium levels at baseline, then again at 2 and 4 weeks after any major dietary change. Some guidelines even recommend testing every 3-6 months if you’re on long-term ACE inhibitors or ARBs.
There’s also a new option for people who need both potassium-rich diets and RAAS inhibitors: patiromer (Veltassa). It’s a potassium binder - it traps excess potassium in your gut so your body doesn’t absorb it. Clinical trials show it keeps potassium in the safe range for 89% of patients who previously struggled.
What About Supplements?
Don’t take potassium supplements unless your doctor prescribes them. Even over-the-counter pills can be dangerous. A 2017 study found that patients with chronic kidney disease who took potassium chloride supplements had an 11% chance of developing dangerous hyperkalemia - even with normal kidney function.Dietary potassium from whole foods is safer because your body absorbs it slowly. Supplements dump a large dose into your system all at once. That’s why the American Heart Association and the FDA both warn against potassium supplements for people on blood pressure meds.
The Bigger Picture
Most Americans eat only about 2,400 mg of potassium a day - less than half the recommended amount. That’s one reason why high blood pressure is so common. But the solution isn’t just “eat more potassium.” It’s “eat more potassium - safely.”Public health campaigns like the AHA’s “Power Up” initiative are trying to fix this. But they’re also learning that blanket advice doesn’t work. You can’t tell someone on spironolactone to eat a banana for breakfast and a spinach salad for lunch without checking their labs first.
The future of blood pressure care is personalized. New tools like Omron’s HeartGuide smartwatch - launching in mid-2024 - will let you track potassium trends over time. But right now, the best tool you have is your doctor, your lab results, and your food log.
Bottom Line
High-potassium foods are great for lowering blood pressure - if your kidneys and meds can handle them. But if you’re on ACE inhibitors, ARBs, or potassium-sparing diuretics, you’re playing with fire if you don’t monitor your intake.Don’t panic. Don’t stop eating vegetables. Just get tested. Track your meals. Talk to your doctor. And don’t assume that what’s healthy for one person is safe for you.
Your blood pressure might drop. Your heart might thank you. But your kidneys need to be in the loop - or this could go very wrong.
Can I eat bananas while taking lisinopril?
You can eat bananas, but only in moderation - one per day is usually fine if your potassium levels are normal. If your potassium is already above 4.8 mmol/L, even one banana could push you into danger. Always check your blood levels before making dietary changes. Many patients on lisinopril switch to lower-potassium fruits like apples, berries, or grapes to stay safe.
Is potassium salt substitute safe with blood pressure meds?
No, not if you’re on ACE inhibitors, ARBs, or potassium-sparing diuretics. These substitutes contain potassium chloride and can raise your blood potassium by 0.3-0.5 mmol/L - enough to trigger hyperkalemia. Even small amounts, like a pinch on your food, add up. Stick to regular salt or sodium-free seasonings without potassium.
How often should I get my potassium checked?
If you’re starting a new blood pressure med like lisinopril or losartan, get tested at baseline, then again at 2 and 4 weeks. After that, if your levels are stable, every 3-6 months is standard. If you have kidney disease or are over 65, your doctor may recommend testing every 3 months. Never skip these tests - high potassium has no early warning signs.
What are the safest high-potassium foods if I’m on blood pressure meds?
There aren’t truly “safe” high-potassium foods if you’re on potassium-retaining meds - it’s about portion control and balance. Instead of large servings of spinach or sweet potatoes, try smaller portions mixed with low-potassium foods. For example, 1/2 cup cooked spinach (420 mg) with white rice and grilled chicken is safer than a full cup. Focus on variety and moderation, not elimination.
Can I stop my blood pressure meds if I eat more potassium?
Never stop your meds without talking to your doctor. While potassium can help lower blood pressure, it doesn’t replace medication for most people. Stopping your pills suddenly can cause dangerous spikes in pressure. The goal is to combine diet and meds safely - not to replace one with the other.
Does kidney disease change how I should handle potassium?
Yes - significantly. If your eGFR is below 60, your kidneys can’t clear potassium well. You’re at much higher risk for hyperkalemia, even with normal dietary intake. Many doctors limit potassium-rich foods in patients with advanced kidney disease. Always get your kidney function tested and follow your nephrologist’s advice. Supplements and salt substitutes are especially dangerous in this group.
What should I do if I feel muscle weakness or heart palpitations?
Call your doctor immediately or go to urgent care. These could be early signs of hyperkalemia. Don’t wait to see if it passes. A simple blood test can confirm your potassium level. If it’s above 5.5 mmol/L, you may need emergency treatment to lower it. Delaying care can lead to cardiac arrest.
Are there apps to track potassium intake?
Yes. The National Kidney Foundation’s “Potassium Counts” app is free and widely used. Cronometer is another reliable option that lets you log meals and track potassium alongside sodium and other nutrients. These apps help you spot patterns - like how your potassium spikes after eating a large salad or drinking coconut water. Tracking for just a week can reveal hidden risks.




Nicholas Miter
January 26, 2026 AT 04:27Been on lisinopril for 5 years. Ate a banana every morning like it was gospel. Got my labs done last year - potassium was 5.4. Didn’t feel a thing. Went to the ER after a weird flutter in my chest. Turned out I was one avocado away from a cardiac event. Now I swap bananas for apples. No drama. No meds changed. Just smarter eating.
Josh josh
January 28, 2026 AT 02:34bro just stop using salt substitutes theyre literally potassium bombs in a shaker
Sally Dalton
January 29, 2026 AT 07:31Thank you for this. I’m on losartan and just started eating more veggies because everyone says it’s healthy. I had no idea I could be poisoning myself without knowing it. I’m going to get my levels checked tomorrow. I feel so much better knowing what to look out for now 💙
Shawn Raja
January 30, 2026 AT 16:42Oh so now we’re blaming bananas? Next they’ll say sunlight causes cancer because it gives you vitamin D. The real problem isn’t potassium - it’s lazy doctors who don’t monitor their patients. If your med makes you vulnerable to a fruit, maybe the med’s the problem, not the diet. Also, coconut water is not a drug. Chill.
Suresh Kumar Govindan
January 31, 2026 AT 11:08The pharmaceutical-industrial complex has conditioned you to fear natural substances. Potassium is a fundamental electrolyte. The fact that synthetic drugs interfere with it is not a failure of nutrition - it is a failure of pharmacology. You are being manipulated into believing food is dangerous. This is not medicine. It is control.
Joanna Domżalska
February 1, 2026 AT 08:43so you’re telling me eating healthy can kill you? what a joke. next they’ll say breathing is dangerous if you’re on a beta blocker. this is fearmongering dressed up as advice. if your body can’t handle potassium, maybe you shouldn’t be on that med. fix the drug, not the diet.
Rakesh Kakkad
February 2, 2026 AT 22:05As a physician practicing in Mumbai, I have seen too many patients on ACE inhibitors consume large quantities of coconut water, spinach, and salt substitutes under the mistaken belief that they are 'healthy.' The consequences are not theoretical - I had a 68-year-old man present in ventricular fibrillation after a week of daily coconut water and potassium chloride seasoning. This is not anecdotal. It is clinical reality. Always test. Always monitor. Never assume.
Henry Jenkins
February 3, 2026 AT 15:56There’s a deeper issue here that nobody’s talking about. We treat blood pressure like it’s a single variable to be optimized, when it’s actually a system-wide imbalance. Potassium isn’t the villain - our entire food system is. We’re told to eat more plants, then told not to eat the plants that have the most nutrients because they interfere with drugs designed to compensate for our bad diet. It’s a loop. The real solution isn’t swapping spinach for lettuce - it’s fixing the upstream causes of hypertension: stress, processed food, sedentary lifestyles, and healthcare that treats symptoms, not root causes. But that’s too expensive for Big Pharma, so we get banana warnings instead.
Dan Nichols
February 5, 2026 AT 05:07People who don’t read the label deserve what they get. If you’re on spironolactone and you’re eating a banana smoothie with potassium salt and avocado toast you’re not being healthy - you’re being stupid. The warning is right there in the patient info sheet. This isn’t rocket science. Stop blaming the system. Take responsibility.
Ryan W
February 5, 2026 AT 21:46USA healthcare is a joke. In Germany, every patient on RAAS inhibitors gets automatic potassium testing at 14 days. Here? You’re lucky if your PCP remembers your name. This post should be mandatory reading for every primary care doctor in America. But they’re too busy pushing prescriptions to bother with actual care.
eric fert
February 6, 2026 AT 18:29Let me tell you what’s really happening. The FDA approves drugs that cause hyperkalemia because they’re profitable. Then they tell you to avoid potassium-rich foods - not because it’s dangerous, but because they don’t want to admit the drug is flawed. They profit from the drug AND the lab tests AND the binders like Veltassa. It’s a triple revenue stream. You’re not being helped - you’re being monetized. The truth? Potassium isn’t the problem. The profit motive is.
Napoleon Huere
February 8, 2026 AT 16:24There’s a philosophical paradox here. We’re told to eat clean, whole foods to heal our bodies - yet the very tools we use to heal (medications) make those same foods dangerous. Are we meant to be in conflict with nature? Or is medicine just a temporary patch on a broken system? I don’t have answers. But I do know this: if your health depends on avoiding a banana, something is deeply wrong with how we define wellness.
Aishah Bango
February 9, 2026 AT 07:37People like you who say 'just get tested' are part of the problem. Testing doesn’t fix the system. It just makes you feel better about being complicit. The real solution is to stop prescribing drugs that turn food into poison. Why not try lifestyle medicine first? Why not teach people to eat real food and move their bodies? Instead we hand out pills and then act shocked when people die from eating spinach. It’s not patient error - it’s medical arrogance.
Geoff Miskinis
February 10, 2026 AT 23:28Of course the American Heart Association says potassium is good. They’re funded by pharmaceutical companies that sell potassium binders. The same people who profit from your hyperkalemia are the ones telling you what to eat. The data is skewed. The guidelines are conflicted. Don’t trust institutions. Trust your own labs. And never, ever trust a salt substitute.
Allie Lehto
February 11, 2026 AT 03:21i just found out my dad died from this and no one told him. he was on lisinopril and ate like 3 bananas a day because he thought he was being healthy. he never got his levels checked. he just got weaker and weaker until he couldn't stand. i hate that no one warned him. please if you're reading this and on one of these meds - get tested. don't wait. i'm crying right now typing this.