Every year, millions of people in the U.S. take vitamins, herbs, or protein powders without telling their doctor. They think it’s harmless-just a little extra support for energy, sleep, or immunity. But what if that daily turmeric capsule is quietly reducing the power of your blood thinner? Or that ginkgo biloba you take for memory is making you bleed more than you should? These aren’t rare accidents. They’re predictable, preventable, and happening right now.
Why This Isn’t Just a ‘Maybe’ Risk
You’ve probably heard that supplements are ‘natural,’ so they must be safe. That’s the myth. The truth? Dietary supplement-drug interactions are a quiet public health issue. In 2023, the FDA received over 1,800 reports of adverse events tied to supplements mixing with medications. Warfarin, the blood thinner, was involved in more than a third of those cases. St. John’s wort, a popular herb for mood, was linked to nearly 30% of all serious interactions tracked by the Natural Medicines Database.
Here’s the problem: supplements don’t go through the same testing as prescription drugs. Under the Dietary Supplement Health and Education Act (DSHEA) of 1994, manufacturers don’t need to prove safety or effectiveness before selling. The FDA can only act after harm occurs. That means if a supplement causes a dangerous interaction, it’s already on store shelves, in your medicine cabinet, and possibly in your body.
How Supplements and Drugs Actually Clash
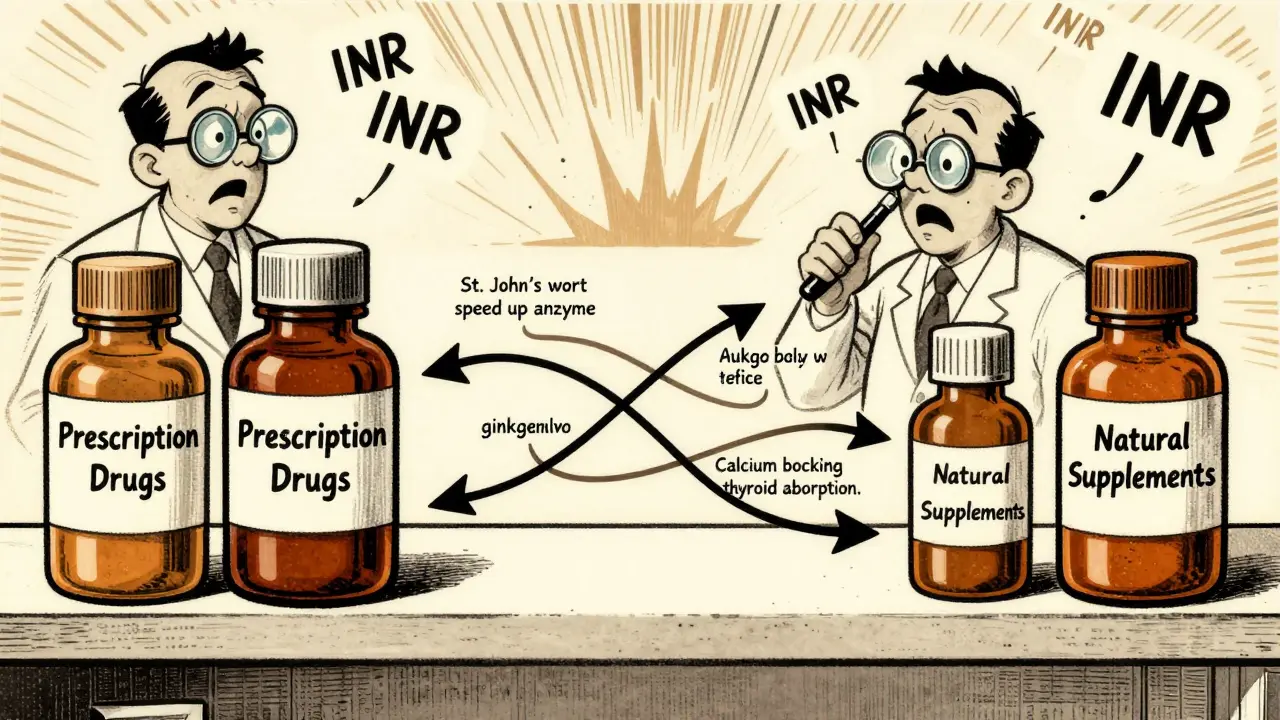
Interactions happen in two main ways-either by changing how your body handles the drug, or by changing how the drug works in your system.
Pharmacokinetic interactions affect how your body absorbs, breaks down, or gets rid of a drug. For example, St. John’s wort speeds up a liver enzyme called CYP3A4. This enzyme is responsible for breaking down more than half of all prescription drugs. When it’s overactive, drugs like cyclosporine (used after transplants), indinavir (for HIV), and even birth control pills get cleared too fast. Studies show cyclosporine levels can drop by 57%-enough to cause organ rejection.
Pharmacodynamic interactions change how a drug acts in your body. Ginkgo biloba and garlic both thin the blood. When taken with warfarin, they don’t just add to the effect-they multiply it. Case reports show INR levels (a measure of blood clotting) jumping from a safe 2.5 to over 6.5. That’s a 150% increase in bleeding risk. One patient needed emergency surgery after a brain bleed.
Even something as simple as calcium can interfere. If you take levothyroxine for hypothyroidism and a calcium supplement at the same time, your body absorbs up to half less of the thyroid hormone. That means you’re not getting the full dose-even if you’re taking it exactly as prescribed.
High-Risk Supplements You Should Know
Not all supplements are equal when it comes to risk. Some are harmless with most medications. Others? They’re ticking time bombs.
- St. John’s wort: Avoid with antidepressants (SSRIs, SNRIs), blood thinners, birth control, HIV meds, and seizure drugs. It’s the most common culprit in serious interactions.
- Ginkgo biloba: High risk with warfarin, aspirin, and NSAIDs. Increases bleeding, even at low doses.
- Green tea extract: High in vitamin K. Can make warfarin useless. Don’t take it if you’re on blood thinners.
- Magnesium: Found in antacids and some multivitamins. Blocks absorption of antibiotics like ciprofloxacin and levofloxacin. Take them at least 2 hours apart.
- Cranberry: Once thought to be safe with warfarin, but newer studies show it can increase bleeding risk. Still debated, but better to avoid if you’re on blood thinners.
- Red yeast rice: Contains lovastatin-a statin drug. Mixing it with other statins or fibrates can cause rhabdomyolysis, a life-threatening muscle breakdown.
- CBD oil: Can spike levels of clobazam (an anti-seizure drug) by up to 500%. Also interferes with blood thinners and some antidepressants.
On the other hand, supplements like American ginseng, milk thistle, and saw palmetto have very low interaction risk based on current data. But “low risk” doesn’t mean “no risk.” Always check.
Who’s Most at Risk?
It’s not just older adults taking five prescriptions. It’s anyone who takes more than one medication and a supplement-even if it’s just “one capsule a day.”
People over 60 are the most vulnerable. Nearly 85% of them take supplements, and most are on 4-5 prescription drugs. That’s a perfect storm for interactions. A 72-year-old on warfarin, lisinopril, and atorvastatin who starts taking fish oil and CoQ10 might not feel anything right away. But over time, the fish oil thins the blood, CoQ10 slightly reduces statin effectiveness, and the warfarin becomes harder to control.
Patients with chronic conditions-heart disease, diabetes, epilepsy, cancer-are especially at risk. Their medications are narrow-therapeutic-index drugs. That means the difference between the right dose and a toxic dose is tiny. Even a 10% change in blood levels can cause serious harm.
Why Patients Don’t Tell Their Doctors
Studies show 43% to 69% of patients never mention their supplements to their doctors. Why?
- “My doctor doesn’t know anything about supplements anyway.”
- “I didn’t think it mattered.”
- “I bought it at the health food store-it’s natural.”
- “I didn’t want to sound like I was ignoring advice.”
Reddit threads from 2020 to 2023 show that 68% of users never discussed supplement use with their providers. One user wrote: “I told my cardiologist about my fish oil. He just nodded and said, ‘Keep taking it.’ I didn’t realize it could interfere with my blood thinner.”
Doctors aren’t always to blame. A 2020 study found only 32% of pharmacists could correctly identify major supplement-drug interactions. After a 4-hour training course, that jumped to 87%. The knowledge gap isn’t just in patients-it’s in the system.
What You Can Do Right Now
You don’t need to stop supplements. You just need to be smart about them.
- Make a list. Write down every supplement you take-name, dose, frequency. Include herbal teas, protein powders, and CBD oils.
- Bring it to every appointment. Don’t wait for them to ask. Say: “Here’s what I’m taking besides my prescriptions.”
- Ask two questions: “Could this interact with any of my medications?” and “Is there a safer alternative?”
- Use trusted resources. Check the Natural Medicines Database or NIH’s LiverTox. Avoid random blogs or YouTube videos.
- Time your doses. If you take calcium or magnesium, take it 2-4 hours apart from antibiotics or thyroid meds.
- Report bad reactions. If you feel unusual bruising, dizziness, or bleeding after starting a new supplement, report it to the FDA’s MedWatch program.
The Bigger Picture
The U.S. supplement market is worth over $52 billion. By 2028, it’s expected to hit $83 billion. But only 12% of manufacturers do formal interaction testing. Labels rarely warn about risks. And the FDA can’t stop a dangerous product until someone gets hurt.
That’s why experts like Dr. Pieter Cohen from Harvard call the current system “a public health failure.” He points to red yeast rice supplements that contained unlisted lovastatin-causing muscle damage in people already on other cholesterol drugs. These weren’t accidents. They were predictable.
Legislation like the 2023 Dietary Supplement Labeling Act (H.R.2409) is pushing for mandatory interaction warnings on high-risk products. The NCCIH has committed $15.7 million to research through 2025. But until those changes happen, the burden is on you.
Final Thought: Safety Isn’t About Avoiding Supplements
It’s about knowing what you’re mixing. Supplements aren’t the enemy. Ignorance is.
If you’re on blood thinners, antidepressants, transplant meds, or seizure drugs-your supplement routine needs a safety check. Don’t assume it’s fine because it’s “natural.” Don’t wait for your doctor to ask. Be the one who speaks up. Keep your list. Ask the questions. Protect yourself.
Because in the end, your health isn’t just about what you take-it’s about what you know.




Jackie Be
December 20, 2025 AT 12:22I took ginkgo for months and never knew it could make me bleed like a stuck pig
Jon Paramore
December 20, 2025 AT 15:28Pharmacokinetic interactions via CYP3A4 induction are the silent killers here. St. John’s wort isn’t just ‘natural’-it’s a potent enzyme inducer. Cyclosporine levels dropping 57%? That’s not anecdotal-it’s pharmacologically inevitable. Most patients have zero awareness of hepatic metabolism pathways. The FDA’s reactive model is a disaster.
John Hay
December 21, 2025 AT 01:03My mom took turmeric with her blood thinner. She ended up in the ER with a hematoma the size of a grapefruit. Doctors never asked. She never thought to tell them. This needs to be on every bottle.
Cara C
December 22, 2025 AT 23:23It’s not about fear-it’s about awareness. I started keeping a little notebook of everything I take, even the herbal tea. I bring it to every appointment now. My pharmacist actually thanked me. Small steps matter.
Siobhan K.
December 23, 2025 AT 16:50Of course the FDA doesn’t regulate supplements-because the industry funds their lobbying. You think this is an accident? It’s business. $52 billion and counting. Natural doesn’t mean safe. It means unregulated and profitable.
Adrian Thompson
December 23, 2025 AT 23:03They’re hiding the truth. The FDA knows what’s happening. They let it slide because Big Pharma wants you dependent on pills. Supplements are the real medicine. They’re scared you’ll wake up and stop taking their toxic drugs.
Stacey Smith
December 25, 2025 AT 22:31Americans are dumb. You take some random herb from a store and wonder why you’re dizzy? Read the label. Or better yet-don’t take anything unless your doctor says so. We’re not lab rats.
Sandy Crux
December 26, 2025 AT 18:24...and yet, you’re all so eager to reduce complex pharmacological phenomena to simplistic, fear-driven bullet points... as if the body is a mechanical system that responds predictably to isolated variables... how profoundly reductionist... how tragically modern...
Orlando Marquez Jr
December 27, 2025 AT 01:35As a healthcare professional with over two decades of clinical experience, I must emphasize that the absence of regulatory oversight does not equate to absence of risk. The burden of patient education remains disproportionately placed on clinicians who are neither trained nor compensated to address dietary supplement pharmacology in routine practice. This is a systemic failure requiring policy intervention, not merely individual vigilance.
Erika Putri Aldana
December 28, 2025 AT 13:10lol why do people even care? just take your pills and your gummies and if you die, you die. it’s not like the world needs more overeducated hypochondriacs. 🤷♀️
Cameron Hoover
December 29, 2025 AT 12:21I used to think supplements were just for people who didn’t trust modern medicine. Then I found out my dad’s heart meds were being weakened by his CoQ10. He’s fine now. Just didn’t know. That’s the real tragedy-not the supplement. It’s the silence.
Michael Ochieng
December 30, 2025 AT 05:22My cousin in India takes ashwagandha with his BP meds. No issues. Maybe it’s not the supplement-it’s the American obsession with dosing everything to the milligram. We’ve lost touch with balance.
Theo Newbold
December 31, 2025 AT 22:08Let’s be real. The only reason this is a ‘problem’ is because people don’t read the fine print. If you’re taking 7 different things and don’t know how they interact, you’re not a victim-you’re negligent. The system isn’t broken. You are.
Swapneel Mehta
January 1, 2026 AT 10:01I live in India and we’ve been using turmeric, neem, and ashwagandha for centuries. But we also know our bodies. We don’t mix them with Western meds without a local practitioner. Maybe the answer isn’t banning supplements-it’s teaching cultural pharmacology alongside medical training.