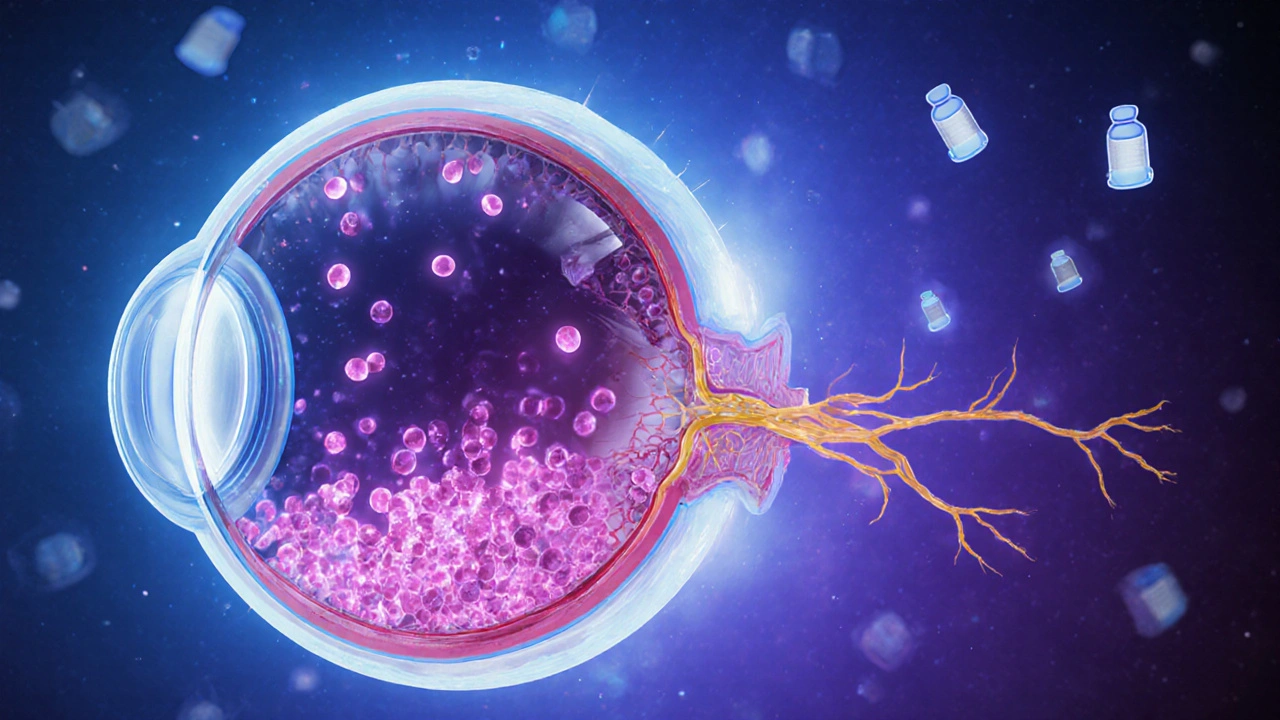
Open-Angle Glaucoma is a chronic eye disease marked by progressive loss of optic nerve fibers, usually linked to elevated intraocular pressure. It is the most common form of glaucoma worldwide, affecting over 60 million people. Diabetes Mellitus is a metabolic disorder where high blood sugar levels damage blood vessels and nerves throughout the body, including the eye. In 2024, the International Diabetes Federation estimated 537 million adults living with diabetes.
Why Diabetes Matters for Eye Health
People often associate diabetes with diabetic retinopathy, but the disease’s impact goes far beyond the retina. Chronic hyperglycemia (HbA1c levels above 7%) leads to microvascular dysfunction, oxidative stress, and inflammation. These processes disturb the delicate balance of fluid dynamics inside the eye, setting the stage for glaucoma.
Pathophysiological Links Between Diabetes and Open-Angle Glaucoma
Three main mechanisms connect the two conditions:
- Vascular Complications: Diabetes impairs blood flow to the optic nerve head, reducing oxygen delivery and making nerve fibers more vulnerable to pressure‑related damage.
- Elevated Intraocular Pressure (IOP): Studies show diabetic eyes often have higher Intraocular Pressure due to reduced outflow through the trabecular meshwork, which can be thickened by glycation end‑products.
- Neurodegeneration: Independent of pressure, high glucose levels trigger apoptosis of retinal ganglion cells and thinning of the Retinal Nerve Fiber Layer, a hallmark of early glaucoma.
These pathways often overlap, meaning a diabetic patient may develop glaucoma even with normal IOP readings, a condition sometimes called "normal‑tension glaucoma."
Epidemiological Evidence: Numbers That Speak
Large‑scale cohort studies consistently report a higher incidence of open‑angle glaucoma among diabetics:
- A 2022 Meta‑analysis of 15 prospective studies found a 1.4‑fold increased risk (RR=1.38, 95%CI1.23‑1.55) for those with Type2 diabetes.
- The UK Biobank data (over 500,000 participants) showed that each 1% rise in HbA1c was associated with a 3% uptick in glaucoma odds.
- In Asian populations, where primary open‑angle glaucoma is prevalent, diabetic patients exhibited a 2‑year earlier onset on average.
These figures underscore that diabetes is not a peripheral risk factor; it is a central driver of glaucoma prevalence.
Clinical Signs & Screening Tools
Because diabetes can mask typical pressure‑related clues, comprehensive eye exams become essential.
- Measure Intraocular Pressure using Goldmann applanation tonometry.
- Assess optic nerve head health with fundus photography and Optical Coherence Tomography (OCT) to quantify Retinal Nerve Fiber Layer thickness.
- Perform automated visual field testing to detect functional loss.
- Review systemic control: recent HbA1c results and blood pressure readings.
For diabetic patients, the American Academy of Ophthalmology recommends an eye exam at diagnosis, then annually thereafter.
Management Strategies Tailored for Diabetic Patients
Treating glaucoma in the context of diabetes involves a dual focus: lowering eye pressure and optimizing systemic health.
- Medication Choices: First‑line Antiglaucoma Medication (e.g., prostaglandin analogues) are generally safe for diabetics. However, beta‑blockers may affect blood glucose regulation, so clinicians often prefer preservative‑free formulations.
- Laser & Surgical Options: Selective laser trabeculoplasty (SLT) can reduce IOP without systemic side effects. In advanced cases, micro‑invasive glaucoma surgery (MIGS) offers a safer profile for patients with co‑existing vascular disease.
- Glycemic Control: Tight blood sugar management (HbA1c<7%) slows retinal nerve fiber loss, as shown in the DCCT/EDIC follow‑up studies.
- Blood Pressure & Lipids: Hypertension exacerbates optic nerve ischemia. Statin therapy has been linked to modest IOP reduction, presenting a synergistic benefit.
Regular coordination between endocrinologists and ophthalmologists ensures that medication side effects and disease progression are monitored holistically.
Prevention and Lifestyle Recommendations
Beyond medical therapy, everyday habits can buffer the diabetic‑glaucoma link:
- Exercise: Moderate aerobic activity improves insulin sensitivity and may lower IOP by enhancing aqueous outflow.
- Diet: A Mediterranean‑style diet rich in omega‑3 fatty acids, leafy greens, and low‑glycemic index foods supports vascular health.
- Avoid Smoking: Tobacco worsens microvascular damage and is associated with higher glaucoma incidence.
- Stay Hydrated, but Moderately: Rapid fluid ingestion can cause transient IOP spikes; sipping water throughout the day is preferable.
These measures echo advice from the American Diabetes Association and the National Eye Institute, reinforcing that lifestyle is a frontline defense.
Key Takeaways
In short, diabetes amplifies the risk of open-angle glaucoma through vascular, pressure‑related, and neurodegenerative pathways. Early detection via comprehensive eye exams, vigilant blood‑sugar control, and individualized glaucoma therapy can preserve vision for the long term.
| Population | Incidence (per 1,000 person‑years) | Average Age at Diagnosis | Mean HbA1c (if applicable) |
|---|---|---|---|
| Adults with Diabetes | 3.2 | 58 | 7.8% |
| Adults without Diabetes | 2.1 | 63 | N/A |
Related Topics You Might Explore Next
Understanding the diabetes‑glaucoma link opens doors to other eye‑health subjects. Consider reading about:
- Diabetic Retinopathy: screening protocols and treatment advances.
- Normal‑Tension Glaucoma: when pressure isn’t the main culprit.
- Impact of Systemic Hypertension on Optic Nerve Health.
- Emerging Neuroprotective Therapies for Glaucoma.

Frequently Asked Questions
Does having diabetes guarantee I will develop glaucoma?
No. Diabetes raises the risk by roughly 30‑40%, but many diabetics never develop glaucoma. Regular eye exams and good blood‑sugar control dramatically lower that odds.
Can glaucoma cause diabetes?
The relationship is one‑way: diabetes can influence glaucoma development, but glaucoma does not affect glucose metabolism.
Are eye‑drops safe for people with high blood sugar?
Most modern eye‑drops, especially prostaglandin analogues, have no impact on blood sugar. Beta‑blocker drops can sometimes mask hypoglycaemia symptoms, so discuss any concerns with your doctor.
How often should a diabetic get screened for glaucoma?
At diagnosis, a comprehensive dilated eye exam is recommended, followed by annual checks. If additional risk factors (family history, high IOP) exist, your ophthalmologist may suggest more frequent monitoring.
Can lifestyle changes lower my glaucoma risk?
Yes. Maintaining a healthy weight, exercising, eating a balanced diet, and keeping HbA1c below 7% have all been linked to slower optic nerve damage and lower IOP spikes.
What symptoms should prompt an urgent eye visit?
Sudden vision loss, flashes of light, peripheral “shadow” or curtain‑like visual field loss, and unexplained eye pain all require immediate assessment, as they may signal acute glaucoma or retinal events.
Is there a genetic component linking diabetes and glaucoma?
Both conditions have hereditary elements. Certain gene variants (e.g., MYOC, CYP1B1) increase glaucoma risk, while TCF7L2 and others affect diabetes susceptibility. Having a family history of either condition amplifies overall risk.






Christopher Munt
September 26, 2025 AT 17:37Thanks for sharing, very helpful! 😊
Mike Creighton
October 1, 2025 AT 01:00The intertwining of metabolic chaos and ocular pressure reads like a tragic symphony, each chord striking deeper into the optic nerve. When glucose floods the bloodstream, it leaves a silent scar on the trabecular meshwork, subtly raising the intra‑ocular pressure. One can almost feel the relentless push of fluid, a tide that erodes the very fibers that transmit sight. In this drama, the patient becomes both protagonist and victim, navigating a maze of systemic control and local degeneration. It is a stark reminder that diseases do not exist in isolation; they whisper to each other across bodily borders.
Desiree Young
October 5, 2025 AT 08:23This is basic science you should have known by now diabetes makes eyes worse stop ignoring it
Vivek Koul
October 9, 2025 AT 15:47Esteemed readers, it is imperative to recognise the vascular compromise engendered by chronic hyperglycaemia as a pivotal contributor to optic nerve susceptibility. The diminution of perfusion, coupled with glycation‑induced outflow resistance, establishes a milieu conducive to glaucomatous insult. Hence, rigorous glycaemic monitoring must accompany routine tonometric assessments. Furthermore, interdisciplinary collaboration between endocrinologists and ophthalmologists is indispensable for comprehensive care.
Frank Reed
October 13, 2025 AT 23:10Hey, I get where Desiree is coming from but let’s keep it constructive. Diabetes does raise the stakes for glaucoma, that’s a fact. The good news is early screening can catch issues before they become serious. Stay on top of your HbA1c and get those eye exams, it can make a huge difference. Keep pushin forward, you got this!
Bailee Swenson
October 18, 2025 AT 06:33Seriously? This article barely scratches the surface. 🙄 Diabetes isn’t just a footnote, it’s a major driver of ocular disease. If you’re not paying attention to the systemic factors, you’re doing a disservice to patients. 📢
tony ferreres
October 22, 2025 AT 13:56While the data are compelling, we must also consider the philosophical implications of treating a patient as a mere collection of risk factors. 🤔 A holistic view acknowledges the person behind the numbers, yet the urgency to intervene remains. 🚀 The interplay of glucose and pressure is not only physiological but also symbolic of the balance we strive for in medicine.
Kaustubh Panat
October 26, 2025 AT 20:19One must appreciate the intellectual rigor required to dissect such nuanced pathophysiology. The literature unequivocally supports a heightened risk, and to overlook it would be a scholarly misstep. Let us therefore elevate our clinical discourse and prioritize integrated screening protocols.
Arjun Premnath
October 31, 2025 AT 03:42Great point, Frank. Adding to that, collaborative care models have shown success in aligning ophthalmology and endocrinology appointments, reducing missed screenings. Patients benefit from a unified message about the importance of blood sugar control and eye health. Let’s continue encouraging such teamwork.
Johnny X-Ray
November 4, 2025 AT 11:05Absolutely! The optimism in early detection can truly change lives :) Maintaining a positive outlook while managing both conditions is key. Let’s keep spreading awareness and supporting each other through this journey.
tabatha rohn
November 8, 2025 AT 18:28Another oversimplification. The article drifts without depth. 🙁 Diabetes-related glaucoma needs rigorous study, not just a cursory mention.
Mark Rohde
November 13, 2025 AT 01:51What a melodramatic mess! The analysis is as shallow as a puddle after a rainstorm 🌧️. If you want real insight, dig deeper than these surface‑level platitudes.
Rajan Desai
November 17, 2025 AT 09:14Indeed, Mark raises a valid critique. It would be beneficial to explore longitudinal data that quantifies the progression rate of optic nerve thinning in diabetic cohorts. Such granularity could inform more precise screening intervals.
S O'Donnell
November 21, 2025 AT 16:37In considering the extant body of epidemiological evidence, one must take cognizance of the manifold methodological nuances that pervade such investigations. Firstly, the heterogeneity inherent in cohort selection criteria often precipitates variance in risk estimations; a point which, regrettably, is insufficiently addressed in the present composition. Moreover, the omission of granular HbA1c trajectory data precludes a robust correlation analysis between glycaemic volatility and optic nerve degeneration. It is further noteworthy that the discussion omits the potential confounding influence of antihypertensive therapy, a factor with documented ramifications upon intraocular pressure dynamics. The authors' reliance on a meta‑analysis wherein individual study quality is disparate, without judicious weighting, compromises the veracity of the proclaimed 1.4‑fold risk augmentation. Additionally, the discourse fails to contextualise the observed 3% increase per HbA1c percent within a broader therapeutic framework, thereby diminishing its clinical applicability. The neglect of patient‑centred outcomes, such as quality‑of‑life indices, further attenuates the relevance of the findings. Finally, the recommendation for annual ophthalmic examinations, whilst prudent, lacks specificity regarding adjunctive imaging modalities that could augment early detection. In summation, while the article broaches an important intersection of systemic and ocular pathology, the aforementioned methodological lacunae necessitate a more rigorous, stratified analysis to substantiate its clinical imperatives.