Getting your medicine shouldn’t feel like a financial gamble. Yet for millions of people, the price tag on a prescription determines whether they take it-or skip it. Medication adherence isn’t just about remembering to take pills; it’s about being able to afford them. When the cost is too high, people cut doses, delay refills, or skip refills entirely. And the consequences aren’t theoretical-they’re deadly.
In the U.S., about 1 in 10 adults under 65 who take prescription drugs skip or reduce their doses because of cost, according to the CDC. That’s more than 8 million people. Among older adults on Medicare, 1 in 7 say they’ve gone without needed meds because they couldn’t afford them. These aren’t rare cases. They’re systemic. And they’re leading to avoidable hospitalizations, worsening chronic conditions, and around 125,000 deaths each year, as reported by the American Heart Association.
Why Cost Stops People from Taking Their Medicine
It’s not just about the sticker price. It’s about how much you pay out of pocket-copays, coinsurance, deductibles. A study in the American Journal of Managed Care found that when a monthly copay jumped from $10 to over $50, adherence dropped by 15-20%. For someone on multiple medications, that adds up fast. One patient in a Kaiser Health News survey paid $350 a month for her prescriptions after Medicare Part D coverage. That’s more than her monthly rent in some places.
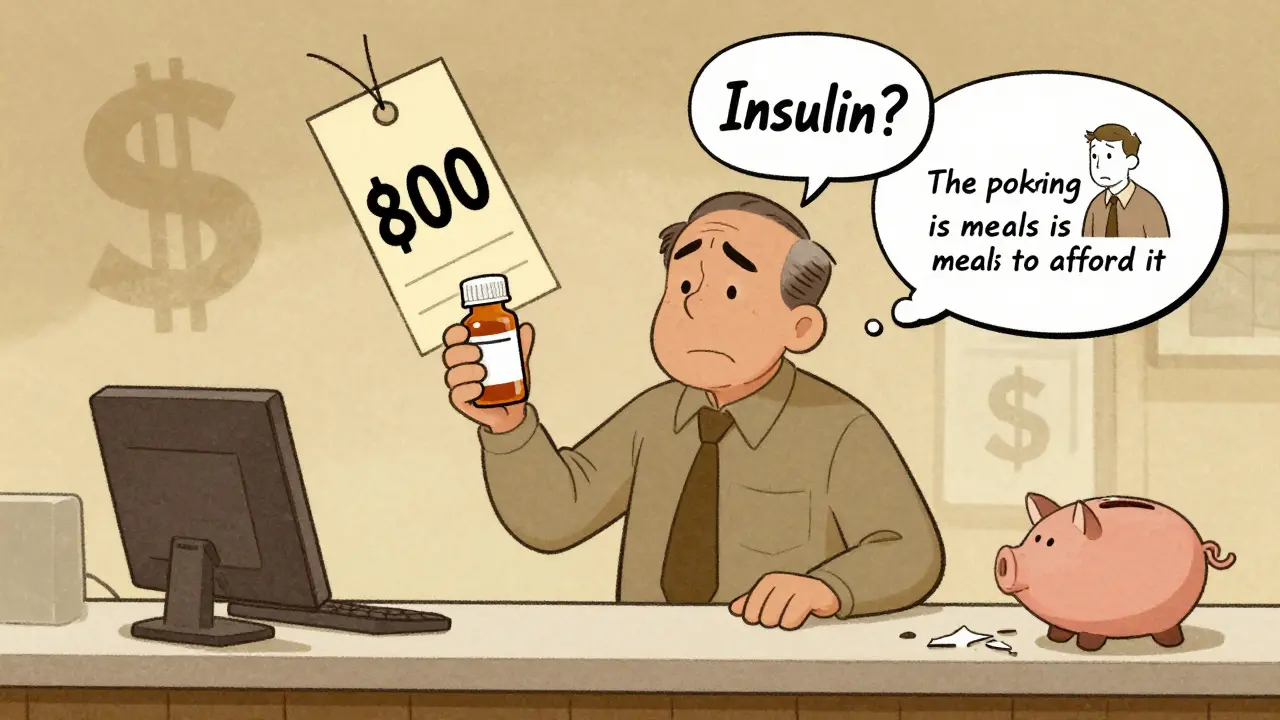
Insulin is the most talked-about example. A 2023 Reddit user shared paying $800 a month for insulin-even with insurance. That’s not an outlier. Between 2007 and 2017, insulin list prices rose 368%, even though the cost to produce it barely changed. People split pills, ration doses, or go without. Some skip meals to pay for meds. Others turn to unregulated online pharmacies. These aren’t choices people make lightly-they’re survival tactics.
Cost barriers hit hardest for people with chronic conditions: heart disease, diabetes, high blood pressure, asthma. These aren’t one-time fixes. These are lifelong treatments. And if you’re making under $25,000 a year, you’re over three times more likely to skip doses than someone making over $75,000, according to CDC data. Women, Black and Hispanic patients, and younger adults are also more likely to face these trade-offs.
What Happens When People Skip Their Meds
Skipping a pill seems harmless. But for someone with high blood pressure, missing doses can spike their risk of stroke. For diabetics, it can mean nerve damage, kidney failure, or amputations. For heart failure patients, it can mean emergency room visits and hospital stays.
The economic toll is just as shocking. Medication non-adherence costs the U.S. healthcare system between $100 billion and $300 billion every year. That’s money spent on avoidable ER trips, hospitalizations, and complications-all because someone couldn’t afford their pills. The American Medical Association calls this a preventable crisis. And it’s not just about individual suffering. It’s about wasted resources, strained systems, and lost productivity.
One 2022 study found that 41% of patients were shocked by the final price at the pharmacy. They thought their insurance covered it. Their doctor didn’t know the cost. That disconnect is common. Prescribers often don’t have real-time access to a patient’s exact copay. That’s changing-but slowly.

How to Get Help: Real Solutions That Work
You don’t have to choose between food and your medicine. There are real, proven ways to cut costs-and they’re not just for the poor.
1. Ask your doctor about alternatives
Your doctor can check if your prescription is on your insurance’s formulary. If it’s not, they can often switch you to a generic version or a cheaper alternative. For example, metformin for diabetes costs less than $10 a month as a generic. Brand-name versions can run $300. Always ask: “Is there a cheaper option that works just as well?”
2. Use GoodRx or SingleCare
These free apps compare prices at local pharmacies. They’re not insurance. They’re coupons. In many cases, they cut the price by 50-80%. A 30-day supply of lisinopril (for blood pressure) might cost $40 at your pharmacy-but $12 with GoodRx. Over 35 million Americans use these tools every month. You don’t need an account. Just show the coupon at the counter.
3. Apply for patient assistance programs
Most big drugmakers have programs that give free or low-cost meds to people who qualify. Eligibility is usually based on income under 400% of the federal poverty level-that’s $55,520 for one person in 2023. These programs helped 1.8 million people in 2022 alone. You can apply directly through the drugmaker’s website or use the Partnership for Prescription Assistance to find the right one. One type 2 diabetes patient went from paying $500 a month for insulin to $25 after enrolling. Her adherence jumped from 60% to 95%.
4. Ask for a 90-day supply
Many insurance plans charge the same copay for a 30-day or 90-day supply. That means you pay less per pill. Mail-order pharmacies often offer this too. Express Scripts reports savings of 20-30% for 90-day fills. It’s one less trip to the pharmacy each month.
5. Use Medicare’s Extra Help program
If you’re on Medicare and have limited income, you may qualify for Extra Help. In 2023, it covered up to $5,000 in annual drug costs. It also reduces your monthly premiums and eliminates the coverage gap (the “donut hole”). Apply through Social Security or your state’s Medicaid office.

What’s Changing in 2025 and Beyond
There’s real momentum for change. The Inflation Reduction Act is making major shifts to Medicare Part D. Starting in 2025, out-of-pocket drug costs for Medicare beneficiaries will be capped at $2,000 a year. The dreaded “donut hole” is gone. And for high-cost drugs, you’ll be able to pay in monthly installments instead of one big bill.
More pharmacies are using real-time benefit tools (RTBTs) that show your exact copay before the prescription is even filled. In 2024, 78% of large health systems plan to use them. But they’re not perfect. A 2022 study found that 37% of estimated prices were off by more than $10. Still, it’s progress.
The FDA approved over 1,100 generic drugs in 2022. That means more competition, lower prices. Insulin prices are finally dropping in some states thanks to new laws. But without nationwide pricing reform, experts warn that 1 in 5 Americans will still skip meds because of cost-even with insurance.
What You Can Do Right Now
If you’re struggling to afford your meds:
- Call your pharmacy and ask for the cash price. It’s often cheaper than your insurance copay.
- Search GoodRx or SingleCare for your drug. Print or show the coupon.
- Ask your doctor: “Is there a generic? Is there a cheaper alternative?”
- Visit pparx.org to find patient assistance programs.
- If you’re on Medicare, call 1-800-MEDICARE and ask about Extra Help.
- Ask for a 90-day supply. Even if you don’t need it all now, you’ll save money long-term.
Don’t wait until you’re sick to act. Talk to your doctor now. Ask for help. There are people who want to support you-not judge you. You’re not alone. And you don’t have to choose between your health and your rent.
Why do people skip their medications because of cost?
People skip or cut doses because out-of-pocket costs like copays, coinsurance, and deductibles are too high. A study found that when copays rose above $50 per month, adherence dropped by 15-20%. Many face impossible choices between medicine, food, rent, or utilities. Even with insurance, some pay hundreds a month for essential drugs like insulin or heart medications.
Is there help for people who can’t afford their prescriptions?
Yes. Pharmaceutical companies offer patient assistance programs that provide free or low-cost medications to those with low income. Apps like GoodRx and SingleCare can cut prices by 50-80%. Medicare beneficiaries may qualify for Extra Help, which covers up to $5,000 in drug costs annually. Asking your doctor for generics or 90-day supplies also reduces costs.
Can I get my medication cheaper with insurance?
Not always. Sometimes the cash price at the pharmacy is lower than your insurance copay. Always ask the pharmacist for the cash price before using insurance. Using discount tools like GoodRx can also beat your insurance rate. Some plans have high deductibles or tiered formularies that make even insured meds expensive.
What should I ask my doctor about medication costs?
Ask: "Is there a generic version?" "Is this drug on my insurance’s formulary?" "Are there cheaper alternatives with the same effect?" "Can I get a 90-day supply?" And don’t be shy: "I’m having trouble affording this. Can we find a solution?" Doctors can often switch you to lower-cost options or connect you with assistance programs.
Are there government programs to help pay for prescriptions?
Yes. Medicare’s Extra Help program assists low-income beneficiaries with Part D costs. The Inflation Reduction Act caps out-of-pocket drug spending at $2,000 per year for Medicare enrollees starting in 2025. Some states also offer prescription assistance programs. Check with your state’s health department or call 1-800-MEDICARE.
What happens if I stop taking my medication because of cost?
Stopping or skipping doses can lead to serious health problems. For heart disease, it raises stroke and heart attack risk. For diabetes, it can cause kidney damage or blindness. For asthma, it can trigger life-threatening attacks. Poor adherence contributes to 125,000 deaths annually in the U.S. and costs the healthcare system up to $300 billion in avoidable care.





Tim Goodfellow
December 20, 2025 AT 23:38Man, this post hit me right in the chest. I’ve seen my uncle ration his insulin like it’s gold-splitting pills, skipping days, crying at the pharmacy counter. It’s not ‘noncompliance,’ it’s survival. And the fact that we let this happen in the richest country on earth? That’s not just broken-it’s evil.
GoodRx saved my mom’s life last year. She was paying $400 for metformin. Found it for $12. She cried. I cried. We didn’t even tell the doctor. Just walked in like ninjas with a coupon.
Elaine Douglass
December 22, 2025 AT 10:43i just wanted to say thank you for writing this. my sister just got diagnosed with hypertension and i was so scared she’d skip her meds because of cost. i showed her goodrx yesterday and she said ‘why didn’t anyone tell me this before?’
we’re gonna call her doc tomorrow and ask about generics. you’re right-we don’t have to choose between food and medicine.
Vicki Belcher
December 24, 2025 AT 00:04THIS. 💔❤️🩹 I’m a nurse and I see this every single day. Patients crying because they’re choosing between their inhaler and their kid’s lunch money. We need systemic change. But until then? Use GoodRx. Ask for 90-day fills. Call the drug company. Don’t be shy. Your life matters more than their profit margins. 💪🩺
Nicole Rutherford
December 25, 2025 AT 12:51People still don’t get it. It’s not that they’re ‘not taking their meds’-it’s that they’re being punished for being poor. You think someone enjoys skipping insulin because they’re lazy? No. They’re terrified. They’re ashamed. And then they get blamed for their own deterioration.
I used to work at a clinic. Saw a woman who gave her insulin to her diabetic husband so he could live. She died of a stroke. She was 38. Her husband still takes his meds. He says he’s ‘paying her debt.’
Don’t pat yourself on the back for using GoodRx. Fix the system. Or at least stop pretending this is about personal responsibility.
Kelly Mulder
December 25, 2025 AT 14:35Let me just say-this is a textbook example of why we need more centralized, state-regulated pharmaceutical pricing. The market-based approach to life-saving drugs is not just morally bankrupt-it’s economically irrational. The fact that a $1 vial of insulin costs $1000 in the U.S. while it’s $10 in Canada is not a ‘market inefficiency.’ It’s corporate malfeasance.
And to those who say ‘just use generics’-yes, that’s a Band-Aid. But the wound is septic. We need price controls. Now.
mark shortus
December 27, 2025 AT 13:19my grandma died because she skipped her heart meds to pay for her insulin. i’m not crying. i’m just… done. 😭
they say ‘there’s help’-but help doesn’t come fast enough. help doesn’t come when you’re gasping in the ER at 3am. help doesn’t come when your kid’s college fund is gone because you paid for a 30-day supply of lisinopril.
we need to burn this system down. not ‘ask your doctor.’ not ‘use GoodRx.’ BURN IT.
Mahammad Muradov
December 27, 2025 AT 14:29Why do people expect free medicine? In India, we pay full price and still take our pills. No coupons. No handouts. Just discipline. If you can’t afford it, you shouldn’t be on it. Life isn’t fair. Get used to it.
bhushan telavane
December 29, 2025 AT 13:18From India, I can say-here, even the poorest take their meds. Why? Because we have no choice. No insurance. No safety net. But we also don’t have $800 insulin. Our government caps prices. Maybe the U.S. should try that instead of telling people to ‘use coupons.’
Also, metformin costs $0.20 a pill here. You pay $300? That’s robbery.
Takeysha Turnquest
December 29, 2025 AT 19:54the system is a mirror. it reflects our collective silence. we let corporations profit off pain because we’re too afraid to look at the faces behind the statistics. we call it ‘healthcare’ but it’s a market. and markets don’t care if you die.
the real question isn’t how to afford meds-it’s how we became okay with this.
Emily P
December 30, 2025 AT 10:52can someone explain how the ‘donut hole’ actually worked? I’ve read about it but I still don’t get how the coverage gap was structured. like, if you hit $4,430 in spending, what exactly happened next? did you pay 100% until you hit catastrophic? just trying to understand.
Jedidiah Massey
December 31, 2025 AT 19:43As a healthcare economist, I must emphasize: the marginal utility of insulin is not linear-it’s exponential in terms of public health ROI. The cost of non-adherence ($300B) dwarfs the marginal cost of production ($1.50/vial). The current pricing model is a classic case of negative externality internalization failure. We need Pigouvian subsidies-statutorily mandated-and real-time benefit integration at the point of sale. GoodRx is a stopgap, not a solution.
Also, 87% of patients who use patient assistance programs report >90% adherence. That’s not anecdotal-it’s statistically significant (p<0.01).