Atrial Fibrillation Diet Checker
This tool helps you assess how well your diet aligns with atrial fibrillation guidelines. Answer a few questions about your daily food and drink choices to get personalized feedback.
Why food matters for atrial fibrillation
Living with Atrial Fibrillation is a type of irregular heart rhythm that can cause palpitations, shortness of breath, and fatigue often feels like a constant juggling act between medication, exercise, and stress management. One piece of the puzzle that many overlook is diet. The right foods can help calm electrical activity in the heart, while the wrong choices may trigger episodes. The atrial fibrillation diet isn’t a fad; it’s built on solid clinical evidence and real‑world patient stories. Below you’ll find a step‑by‑step guide that tells you exactly what to fill your plate with and what to keep off it.
How diet influences heart rhythm
Research from the American Heart Association shows that certain nutrients directly affect the heart’s electrical pathways. For example, high sodium loads increase blood pressure, which in turn raises atrial pressure and promotes fibrillation. Conversely, omega‑3 fatty acids improve cell membrane stability, reducing erratic beats.
Below is a quick snapshot of the mechanisms at play:
- Electrolyte balance: Potassium, magnesium, and calcium act like traffic lights for electrical signals.
- Inflammation control: Chronic inflammation widens atrial tissue, making it more prone to chaotic firing.
- Blood pressure regulation: Elevated pressure stretches atrial walls, creating a fertile ground for AF.
Foods that support a stable rhythm
These foods supply the nutrients mentioned above and have been linked to lower AF recurrence rates.
| Food Group | Why it helps | Serving tip |
|---|---|---|
| Leafy greens (spinach, kale) | Rich in magnesium and potassium, both key electrolytes. | Blend into a morning smoothie or toss in a salad. |
| Berries | High in antioxidants that curb inflammation. | Add a handful to oatmeal or yogurt. |
| Whole grains | Provide steady glucose, preventing spikes that stress the heart. | Swap white rice for brown rice or quinoa. |
| Omega-3 fatty acids (fatty fish, flaxseed) | Stabilize cell membranes and reduce arrhythmic triggers. | Aim for two servings of salmon per week. |
| Mediterranean Diet pattern | Combines all heart‑healthy components in one eating style. | Focus on olive oil, nuts, legumes, and fish. |

Foods to limit or avoid
These items are notorious for aggravating AF symptoms.
- Sodium (processed meats, canned soups) - excess salt spikes blood pressure and atrial stretch.
- Alcohol (wine, spirits) - binge drinking can trigger “holiday heart” episodes.
- Caffeine (energy drinks, strong coffee) - high doses increase heart rate and may provoke ectopic beats.
- Sugar‑sweetened beverages - cause rapid glucose swings that stress cardiac cells.
- Trans fats (fried foods, some margarines) - promote inflammation and arterial stiffness.
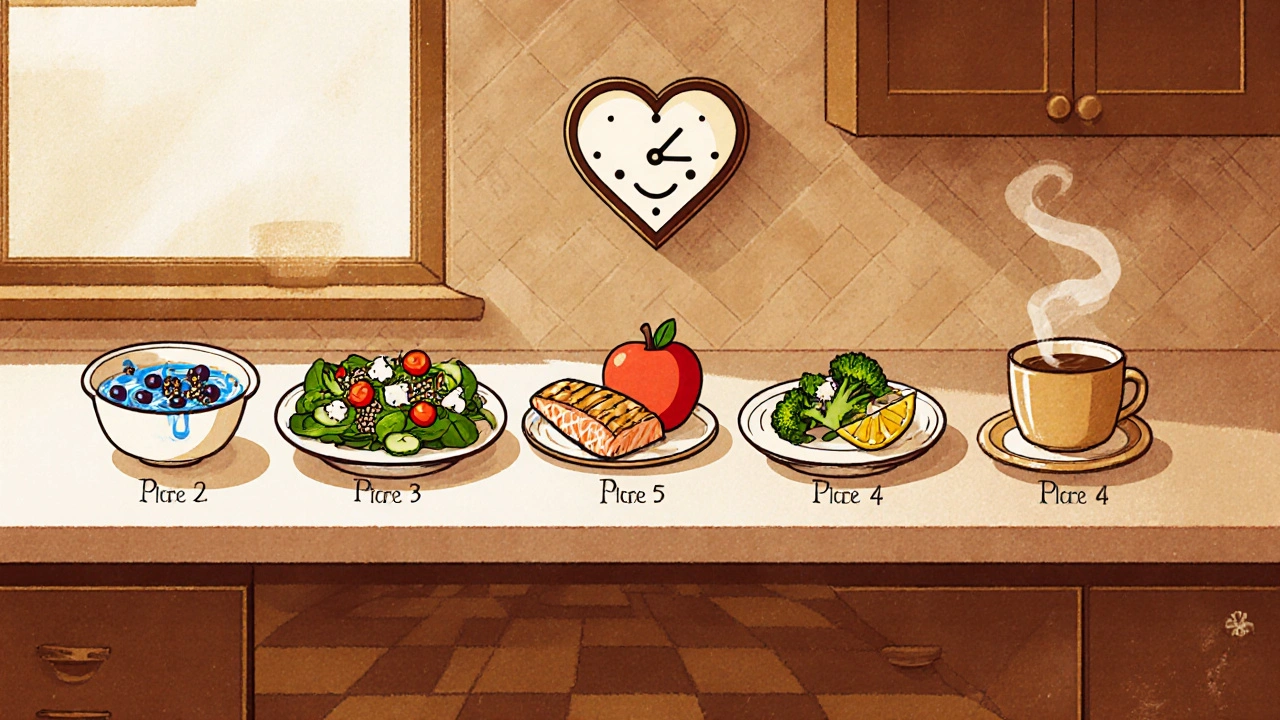
Sample 1‑day meal plan
- Breakfast: Greek yogurt topped with blueberries, a sprinkle of chia seeds, and a drizzle of honey.
- Mid‑morning snack: A small handful of unsalted almonds.
- Lunch: Quinoa salad with spinach, cherry tomatoes, cucumber, feta cheese, and a lemon‑olive‑oil dressing.
- Afternoon snack: Sliced apple with a thin spread of almond butter.
- Dinner: Grilled salmon seasoned with herbs, served with steamed broccoli and sweet potato wedges.
- Evening beverage: Herbal tea (e.g., chamomile) - caffeine‑free.
Notice how the plan leans heavily on omega‑3 rich fish, potassium‑packed greens, and low‑sodium sides. Adjust portions based on your calorie needs and any specific medical advice.
Practical tips for sticking to the plan
- Read labels: Look for “no added salt” or “low‑sodium” tags.
- Cook at home: Home‑cooked meals give you full control over sodium and alcohol.
- Batch prep: Freeze portions of brown rice or quinoa to avoid last‑minute fast‑food grabs.
- Hydrate wisely: Choose water or infused water over soda.
- Track caffeine: Keep intake below 200 mg per day (about one 12‑oz coffee).
When to seek professional guidance
If you’re on anti‑arrhythmic drugs, a dietitian can help avoid nutrient‑drug interactions. For example, grapefruit can interfere with certain calcium‑channel blockers. Also, if you have kidney disease, potassium‑rich foods need careful monitoring.
Frequently Asked Questions
Can a low‑sodium diet really lower AF episodes?
Yes. Studies published in the Journal of the American College of Cardiology show a 15‑20% reduction in AF recurrence when daily sodium intake is kept under 1,500 mg.
Is alcohol completely banned for AF patients?
Moderation is key. Light red wine (one glass) may be acceptable for some, but binge drinking dramatically raises risk. Discuss personal limits with your cardiologist.
How much caffeine is safe?
Most guidelines suggest staying below 200 mg per day - roughly one standard cup of coffee. If you notice palpitations after caffeine, cut back further.
Do supplements like fish oil help?
Clinical trials indicate that 1-2 g of EPA/DHA daily can modestly lower AF burden, especially after cardiac surgery. Always check with your doctor before adding supplements.
What’s the role of potassium‑rich foods?
Potassium counters sodium’s blood‑pressure‑raising effect and supports proper heart electrical function. Bananas, avocados, and beans are excellent sources.
Adopting an atrial fibrillation diet isn’t about strict deprivation-it’s about smarter choices that keep your heart rhythm steady. Start with one or two changes this week, monitor how you feel, and build from there. Your heart will thank you.





Devendra Tripathi
October 21, 2025 AT 00:59The whole “AF diet” hype is overblown; you can live just fine eating what you like as long as you stay active. Cutting every ounce of salt is a marketing ploy not a magic fix. Your heart will beat fine on a regular diet if you keep the meds on schedule. So stop worshipping kale and start listening to your doctor.
Ericka Suarez
October 26, 2025 AT 00:59Wow, this guide is literally a life‑saver! I read it and felt like a new person – the words jump off the page like fireworks. The only thing I cant stand is the lack of bold headings; it could use more drams. But overall its awesome and i totally recommend it to anyone who wants a beat‑steady heart.
Casey Cloud
October 30, 2025 AT 23:59This diet plan hits the core mechanisms that drive atrial fibrillation.
By lowering sodium you reduce atrial pressure which is a primary trigger for irregular beats.
Potassium and magnesium act as natural stabilizers for the electrical impulses.
Whole grains keep glucose levels steady and avoid spikes that stress the heart.
Omega‑3 fatty acids repair cell membranes and calm inflammation.
Leafy greens like kale provide a dense source of magnesium without added calories.
Berries supply antioxidants that combat chronic inflammation in the vascular wall.
The Mediterranean pattern combines these foods with healthy fats for a synergistic effect.
Planning meals ahead of time makes it easier to stick to the low‑salt targets.
Reading labels for “no added salt” can prevent hidden sodium in processed foods.
Cooking at home gives you full control over the ingredients and seasoning.
If you are on anti‑arrhythmic drugs a dietitian can help avoid harmful nutrient interactions.
For patients with kidney issues you may need to monitor potassium intake carefully.
Staying hydrated with water rather than sugary drinks supports electrolyte balance.
Finally track your symptoms and adjust the plan with your cardiologist’s guidance.
Rachel Valderrama
November 4, 2025 AT 23:59Oh sure, just toss out all your coffee and pretend you’re a monk – that’ll totally fix your AF, right? Maybe try actually following the plan for a week before writing a novel about it. Keep that energy, it’s adorable.
Brandy Eichberger
November 9, 2025 AT 23:59Hey there! I love how you’ve laid out the food groups – it’s practically a culinary symphony for the heart. If you sprinkle a bit of olive oil on everything you’ll feel like a gourmet at a five‑star restaurant while keeping rhythm steady. Keep it up!
Eli Soler Caralt
November 14, 2025 AT 23:59i think food is like a poem for the heart 🥬✨ sometimes we miss the rhyme when we over‑salt 🍲 but the universe whispers through berries and fish 🐟💫 ...stay curious, stay balanced 😌
Eryn Wells
November 19, 2025 AT 23:59Everyone can start with small steps – swapping soda for infused water is a win for any palate 🌈. Remember, you’re not alone on this journey; community recipes and shared tips make the path easier 👫. Keep sharing what works for you and we’ll all benefit 😊.
Kathrynne Krause
November 24, 2025 AT 23:59Imagine your heart dancing to the beat of a quinoa‑spinach salad, the rhythm steady and bright! 🌟 Dive into those omega‑rich salmon dinners and feel the pulse of vitality surge through you. Your commitment paints a vivid canvas of health – keep splashing those bold colors onto your plate!
Vivian Annastasia
November 29, 2025 AT 23:59Wow, another “miracle diet” that probably works if you ignore all other medical advice. Seems like a perfect excuse to avoid real treatment while pretending you’re in control. Nice job buying into the hype.
John Price
December 4, 2025 AT 23:59Sure thing.