Drug-Induced Arrhythmia Risk Calculator
Risk Factors Assessment
Answer the following questions to calculate your risk of drug-induced arrhythmias
Many people don’t realize that the very drugs meant to help their heart can sometimes mess it up. Drug-induced arrhythmias are more common than most think - and they can be deadly. Over 400 medications, from common antibiotics to daily pills for depression or high blood pressure, have been linked to abnormal heart rhythms. These aren’t rare side effects. They happen often enough to land tens of thousands of people in the hospital every year in the U.S. alone.
What Exactly Is a Drug-Induced Arrhythmia?
An arrhythmia is when your heart beats too fast, too slow, or irregularly. When it’s caused by a medication, it’s called a drug-induced arrhythmia. This isn’t just about feeling your heart flutter. It’s about real, dangerous changes in the electrical system of your heart. The most serious type is torsades de pointes, a life-threatening ventricular rhythm triggered by prolonged QT intervals on an ECG. This was first noticed in the 1960s with the drug quinidine, and since then, we’ve learned that many more medications can do the same thing.How does this happen? Most drugs interfere with the tiny ion channels in heart cells that control the flow of potassium, sodium, and calcium. When these channels don’t work right, the heart’s rhythm gets thrown off. Some drugs also cause electrolyte imbalances - especially low potassium or magnesium - which makes the problem worse. Even medications you’d never suspect, like certain antihistamines or diabetes pills, can trigger this.
Common Medications That Cause Arrhythmias
You might be surprised to see some of these on your list:- Antibiotics: Macrolides like azithromycin and fluoroquinolones like levofloxacin can prolong the QT interval. Risk spikes in the first week of use.
- Antidepressants and antipsychotics: Drugs like citalopram, sertraline, and haloperidol carry black box warnings from the FDA for QT prolongation. About 12-18% of arrhythmia cases come from these.
- Antiarrhythmics themselves: Ironically, drugs meant to fix arrhythmias - like flecainide, propafenone, and amiodarone - can cause them. Flecainide can turn atrial flutter into a dangerous 1:1 conduction pattern. Amiodarone can cause atrial fibrillation through thyroid dysfunction.
- Digoxin: Used for heart failure and atrial fibrillation, digoxin toxicity (serum levels over 2 ng/mL) causes paroxysmal atrial tachycardia with AV block. Elderly patients with kidney issues are especially at risk.
- Cholesterol drugs: Some statins, especially when combined with other QT-prolonging meds, increase risk.
- Cancer drugs: Trastuzumab (Herceptin) can cause atrial fibrillation in 2-5% of patients by triggering inflammation and oxidative stress in heart tissue.
And here’s something most people miss: multiple drugs together are the biggest red flag. Using two or more QT-prolonging medications can increase arrhythmia risk by 300-500%. That’s not a small jump. It’s a major danger zone.
Who’s Most at Risk?
Not everyone who takes these drugs will have problems. But some groups are far more vulnerable:- Age 65 and older: About 60-70% of severe cases occur in seniors. Their kidneys don’t clear drugs as well, and they often take multiple medications.
- Electrolyte imbalances: Low potassium (hypokalemia) affects 20% of hospitalized patients; low magnesium (hypomagnesemia) hits 10-15%. Both make the heart electrically unstable.
- Excessive alcohol: More than three drinks a day triples your risk. Alcohol messes with potassium levels and directly irritates heart tissue.
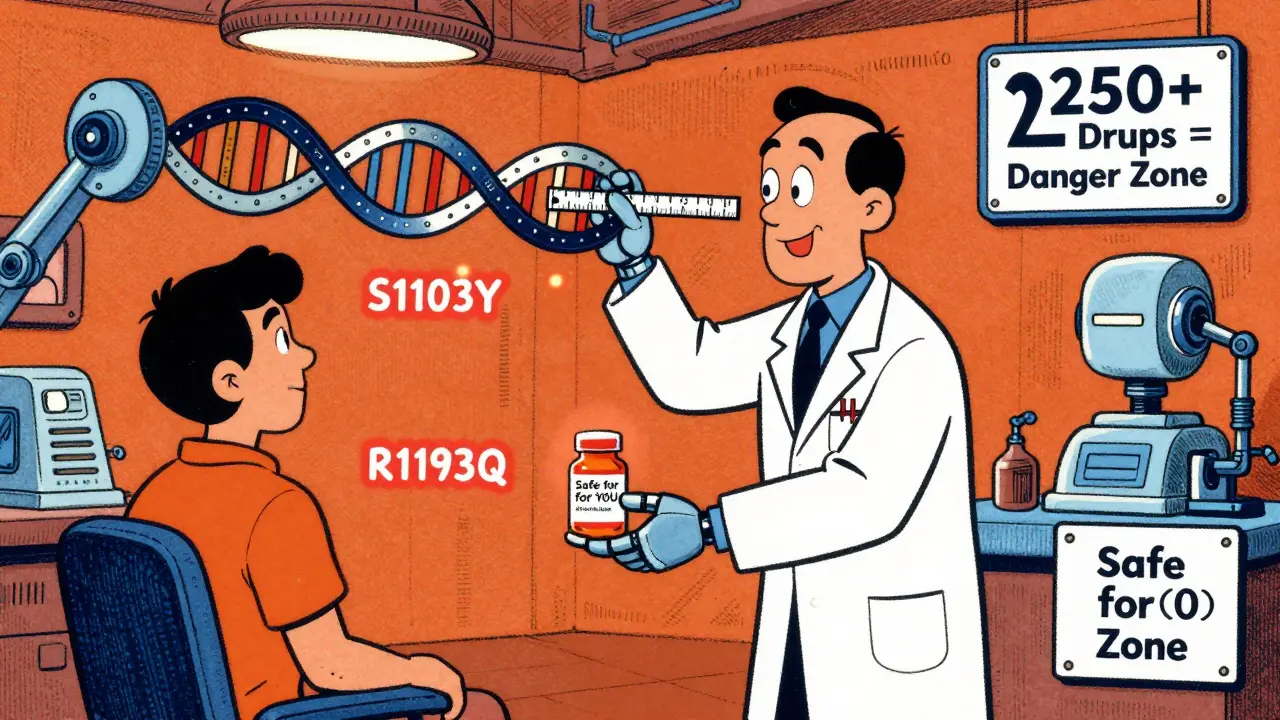
- Genetics: About 15% of people of African ancestry carry the S1103Y variant, and 12% of East Asians carry R1193Q. These gene changes make heart cells way more sensitive to QT-prolonging drugs. Genetic testing is now being studied as a way to prevent these reactions before they start.
Warning Signs You Can’t Ignore
If you’re on any of these meds, pay attention to your body. These symptoms aren’t normal:- Palpitations: Feeling your heart race, skip, or pound - reported by 70-80% of patients.
- Dizziness or lightheadedness: Especially if it happens suddenly or with standing.
- Fatigue: Unexplained tiredness that doesn’t go away with rest.
- Chest discomfort: Not always sharp pain - sometimes just pressure or fullness.
- Fainting or near-fainting: Syncope is a major red flag. About 5-10% of patients with drug-induced arrhythmias experience this.
Don’t brush off dizziness as "just getting older." Don’t think palpitations are "just stress." If you’re on a medication known to affect your heart and you feel any of these, talk to your doctor - don’t wait.
How Doctors Manage These Cases
The good news? Most cases can be fixed without surgery. Here’s how it usually works:- Stop or switch the drug: In 75-85% of cases, simply stopping the offending medication or switching to a safer alternative resolves the arrhythmia.
- Correct electrolytes: Giving IV or oral potassium and magnesium is often the first step. Target levels: potassium above 4.0 mEq/L and magnesium above 2.0 mg/dL.
- ECG monitoring: Before starting high-risk drugs, doctors should do a baseline ECG. Then repeat it within 72 hours. If the QT interval extends more than 60 ms from baseline, the drug should be reconsidered.
- For beta-blocker-induced bradycardia: If your heart rate drops too low (below 50 bpm) and you feel dizzy or weak, reducing the dose helps in 60-70% of cases. If symptoms persist, a pacemaker may be needed - especially if you still need the drug for atrial fibrillation control.
- For persistent cases: Catheter ablation works in 5-10% of patients who don’t respond to meds. Surgery is rare - needed in less than 2%.
It’s not just about stopping the drug. It’s about fixing the environment your heart is in. Low magnesium? Fix it. Dehydrated? Rehydrate. Drinking too much coffee or alcohol? Cut back. These aren’t side notes - they’re part of treatment.
What You Can Do to Protect Yourself
You can’t control everything - but you can control a lot:- Know your meds: Ask your pharmacist or doctor: "Is this drug linked to heart rhythm problems?" Keep a list of everything you take - including OTC drugs and supplements.
- Get an ECG before starting high-risk drugs: Especially if you’re over 65, have kidney disease, or take more than one heart-related medication.
- Monitor your electrolytes: If you’re on diuretics or have chronic conditions like heart failure, ask for regular blood tests for potassium and magnesium.
- Limit caffeine and alcohol: Caffeine causes palpitations in 25-30% of patients. It doesn’t usually cause dangerous arrhythmias alone - but combined with a QT-prolonging drug, it can be the spark.
- Don’t smoke: Smoking damages heart tissue and increases arrhythmia risk.
- Track your symptoms: Keep a simple journal: "On Tuesday, after taking my antibiotic, I felt my heart racing and got dizzy." That’s gold for your doctor.
The Future: Personalized Medicine Is Here
This isn’t just about guessing. Science is catching up. Researchers at Vanderbilt used CRISPR-edited heart cells to prove that people with certain gene variants are far more likely to have dangerous reactions. That means in the near future, doctors may test your DNA before prescribing certain drugs.The American College of Cardiology is rolling out a new clinical tool in 2024 that calculates your personal risk based on age, meds, kidney function, electrolytes, and genetics. It’s not perfect yet - but it’s 75-85% accurate at spotting high-risk patients.
Meanwhile, the FDA has added black box warnings to 25 drugs since 2010 - and 8 of those came in 2022 alone. That shows regulators are finally taking this seriously.
Experts predict that with better screening and smarter prescribing, we could cut severe drug-induced arrhythmias by 30-40% in the next five years. That’s tens of thousands of lives saved.
Final Thought: Don’t Panic - But Don’t Ignore It
Most people who take these medications never have problems. But if you’re in a high-risk group - older, on multiple drugs, with kidney issues, or with a family history of sudden cardiac events - you need to be proactive. Your doctor isn’t always thinking about every possible interaction. You have to be your own advocate.Ask questions. Get tested. Track your symptoms. If something feels off, say something. That simple step could save your life.

Joy F
January 4, 2026 AT 11:24Let’s be real-this isn’t just about meds. It’s about a system that treats your heart like a vending machine: pop in a pill, hope for the best, and pray the machine doesn’t short-circuit. We’ve normalized polypharmacy like it’s a lifestyle brand. And now we’re surprised when the whole damn circuit board catches fire? The FDA’s black box warnings are just PR afterthoughts. Real change would mean mandatory genetic screening before prescribing anything that touches ion channels. But nope-we’d rather let 65-year-olds die quietly while Big Pharma files another quarterly profit report.
And don’t get me started on how doctors dismiss palpitations as "stress." My aunt had three ER visits before anyone checked her QT interval. She was on sertraline, azithromycin, and a diuretic. Three drugs. One perfect storm. She’s fine now. But only because she screamed until someone listened.
This isn’t medicine. It’s Russian roulette with a prescription pad.
Wren Hamley
January 4, 2026 AT 22:04Okay but-what if we flipped the script? Instead of waiting for someone to drop dead from a QT spike, what if every pharmacy printed a little QR code on the bottle that links to a real-time risk calculator? Like, scan it, plug in your age, meds, electrolytes, and boom-you get a color-coded hazard level. Red = don’t take this unless you’ve got a cardiologist on speed dial. Yellow = proceed with caution and get an ECG in 72. Green = go nuts.
I’ve seen people refill antibiotics like they’re candy. No one thinks to ask if it’s gonna make their heart do the cha-cha. We treat meds like coffee-"Oh, I just take it with breakfast." No. This isn’t caffeine. This is tampering with the wiring in your chest. We need better labeling. Not just fine print. Like, bold, blinking, screaming labels.
Also, why isn’t this on the packaging of every OTC antihistamine? Benadryl’s a silent killer. People use it to sleep. That’s not a sleep aid. That’s a cardiac gamble.
Angela Fisher
January 6, 2026 AT 04:48THEY KNOW. THEY KNOW AND THEY DON’T CARE. The pharmaceutical giants have been burying this for decades. Why do you think the FDA only added 8 new black box warnings in 2022? Because the media finally caught wind. But what about the 500+ cases they buried? The ones where people died and the reports got "classified as unrelated"? I’ve seen the leaked emails. One executive wrote: "The risk is statistically insignificant compared to our revenue." STATISTICALLY INSIGNIFICANT? That’s a person. A grandmother. A father. A child.
And the worst part? They’re already testing gene-editing therapies to *fix* the people who survive these reactions. Not to stop the drugs. Not to ban them. To fix the victims. That’s the real horror. They don’t want to prevent this. They want to profit from the aftermath.
They’re selling death as a subscription service. And we’re all signing up.
PS: If you’re on statins + an antibiotic + a diuretic and you’re over 60-STOP. Now. Call your doctor. Don’t wait for your heart to skip. It won’t come back.
Neela Sharma
January 8, 2026 AT 02:13Heart is not just a muscle it is a song
Every pill you swallow is a note in that song
Some notes are gentle like morning breeze
Some are sharp like thunder in a quiet room
When the song becomes a scream
Who do you blame
The medicine
The body
Or the silence between the doctor and the patient
Listen to your heart before it forgets how to sing
It has been whispering all along
Shruti Badhwar
January 8, 2026 AT 03:57While the article provides a comprehensive overview, it fails to address the systemic issue of prescribing inertia. Physicians are often pressured to prescribe within 10-minute visits. The complexity of drug interactions, especially with polypharmacy in elderly patients, is simply not feasible to assess in real time without clinical decision support tools integrated into EHRs. The burden of vigilance is unfairly placed on the patient, who lacks the medical literacy to interpret QT prolongation or electrolyte trends. We need mandatory CDS alerts for high-risk combinations, not just patient education pamphlets. The fact that this is still a manual, reactive process in 2024 is unacceptable. The technology exists. The will does not.
Liam Tanner
January 10, 2026 AT 02:32My dad was on amiodarone for AFib and started feeling dizzy. He thought it was just aging. We didn’t connect it until he passed out in the kitchen. Turned out his potassium was 3.1 and his QT was over 550. They stopped the drug, gave him IV mag, and he’s been fine for two years now. I didn’t know any of this before. I wish someone had told us the signs in plain language-not medical jargon. If you’re on any of these meds, just ask: "Could this make my heart skip?" Don’t wait for a near-death experience to start asking questions. You’re not being difficult. You’re being smart.
veronica guillen giles
January 10, 2026 AT 19:41Oh sweetie. You wrote a 2000-word essay on how drugs can kill you… and you think people are going to read it? Most of us are too busy Googling "why do I feel like I’m dying" at 3 a.m. while swallowing three different pills with a glass of wine. You might as well have printed this on a napkin and left it in the ER waiting room. At least then someone might actually pick it up. Also-did you mention that caffeine + azithromycin + your grandma’s herbal tea = cardiac chaos? No? Then you missed the real epidemic: people treating medicine like a buffet and their heart like a disposable phone.
Angela Goree
January 12, 2026 AT 08:29THIS IS WHY AMERICA IS WEAK!! You people take pills like they’re candy and then wonder why your hearts are falling apart!! We used to be tough! We didn’t need genetic testing to know that if you’re old and on ten drugs, you’re asking for trouble!! You want to live? STOP BEING SOFT!! Quit your coffee! Quit your alcohol! Quit your supplements! Quit your antidepressants if you’re not in a coma!! Stop blaming Big Pharma-STOP BEING LAZY!! My grandfather took digoxin for 30 years and never had a problem because he didn’t whine-he lived!! Get a grip!!
Kerry Howarth
January 13, 2026 AT 19:25Well said. The most important takeaway isn’t the list of drugs-it’s the call to action. If you’re on multiple medications, especially if you’re over 65, get a baseline ECG. Ask for potassium and magnesium levels. Keep a symptom log. These aren’t optional precautions. They’re basic safety checks, like checking your tire pressure before a road trip. You wouldn’t drive a car without knowing if the brakes work. Why treat your heart any differently? This isn’t fearmongering. It’s responsibility. And it’s doable.