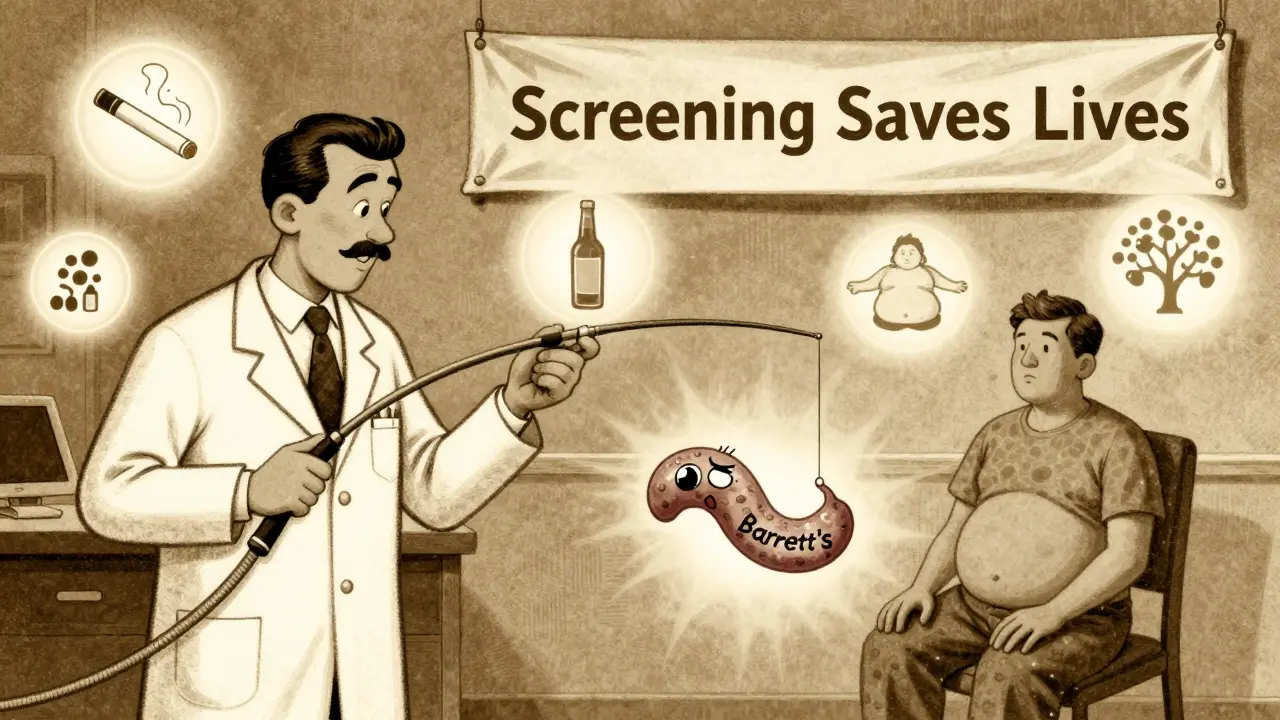
Chronic acid reflux isn’t just a nuisance-it’s a silent warning sign that could lead to cancer. If you’ve had heartburn for five years or more, especially if you’re a man over 50, overweight, or a smoker, you’re not just dealing with discomfort. You’re at risk for a serious condition called esophageal cancer. And the worst part? Most people don’t know they’re in danger until it’s too late.
How GERD Turns Into Cancer
Every time stomach acid backs up into your esophagus, it’s like pouring vinegar on raw skin. Your esophagus isn’t designed to handle that. Over time, the lining starts to change. It thickens. It turns grayish. It starts looking more like the lining of your stomach than your throat. That’s called Barrett’s esophagus. And it’s the only known precursor to esophageal adenocarcinoma-the most common type of esophageal cancer today.This isn’t a quick process. It takes years. Studies show that people with GERD lasting five or more years have a five times higher chance of developing Barrett’s esophagus than those without it. And once Barrett’s is there, the cancer risk doesn’t disappear-it just grows slowly. About 0.2% to 0.5% of people with Barrett’s esophagus develop cancer each year. That sounds small, but when you consider how many people have GERD-nearly 1 in 5 adults in the U.S.-that adds up to thousands of cases annually.
Here’s the twist: most people with GERD never get Barrett’s. Only 10% to 15% of long-term GERD patients do. But if you have other risk factors, your odds jump fast.
The Real Risk Factors
GERD alone isn’t the whole story. It’s the combo that’s deadly. The biggest risk factors aren’t just about how often you get heartburn-they’re about who you are and how you live.- Male sex: Men are 3 to 4 times more likely than women to develop this cancer.
- Age over 50: 90% of cases happen in people over 55. If you’re over 50 and still getting reflux, don’t assume it’s just aging.
- White non-Hispanic ethnicity: White Americans have three times the rate of adenocarcinoma compared to Black Americans.
- Obesity: A BMI over 30 doubles or triples your risk. Fat around your belly pushes stomach contents upward. It’s that simple.
- Smoking: Whether you quit yesterday or 20 years ago, your past smoking history still matters. Smokers have 2 to 3 times the risk.
- Family history: If a parent or sibling had esophageal cancer, your risk goes up.
Combine even two of these with long-term GERD, and your risk becomes serious. For example, a 60-year-old white man with obesity, a 15-year history of reflux, and a smoking past isn’t just at risk-he’s in the high-risk zone. And most people in this group don’t even know they should be screened.
The Red Flags No One Talks About
Heartburn is common. But these symptoms aren’t just bad heartburn-they’re alarms.- Dysphagia: Food getting stuck in your chest or throat. It starts with solids-bread, meat, rice-but soon even liquids feel like they’re catching. This shows up in 80% of people diagnosed with esophageal cancer.
- Unexplained weight loss: Losing 10 pounds or more in six months without trying? That’s not normal. It’s often one of the first signs the cancer is blocking your esophagus or stealing nutrients.
- Chronic hoarseness or cough: If you’ve had a persistent cough or voice change for more than two weeks, especially if you have GERD, it’s not just allergies. Acid can irritate your vocal cords.
- Food impaction: Feeling like food is lodged in your chest for hours after eating. This isn’t indigestion-it’s a physical blockage.
- New or worsening reflux after age 50: If you never had heartburn before, but now you’re getting it daily after turning 50, that’s a red flag. So is reflux that suddenly gets worse after years of being mild.
Here’s what’s scary: 75% of esophageal cancers are found at late stages because people ignore these signs. They think, “It’s just GERD,” or “I’m getting older,” or “I’ll wait and see.” But by the time swallowing becomes hard, the cancer is often advanced.
What You Can Do
The good news? You can stop this before it starts.If you’ve had GERD for five or more years and you’re a man over 50 with one or more other risk factors, talk to your doctor about an upper endoscopy. This is a simple procedure where a thin camera is passed down your throat to check for Barrett’s esophagus. It’s quick, safe, and done under light sedation.
And if Barrett’s is found? Surveillance saves lives. Regular endoscopies every 3 to 5 years can catch early cell changes before they turn cancerous. Studies show this cuts cancer deaths by 60% to 70%.
But screening isn’t enough. Lifestyle changes make a huge difference:
- Quit smoking: Your risk drops by half within 10 years of quitting.
- Lose weight: Shedding just 5% to 10% of your body weight cuts GERD symptoms by 40%.
- Limit alcohol: More than 2 drinks a day for men, or 1 for women, raises risk. Stick to moderate levels.
- Take PPIs as prescribed: If you’re on proton pump inhibitors (like omeprazole or pantoprazole), don’t skip doses. Consistent use for five years reduces cancer risk by 70% in people with Barrett’s esophagus.
And don’t wait for symptoms to get worse. The goal isn’t to manage heartburn-it’s to prevent cancer.
Why This Is Getting Worse
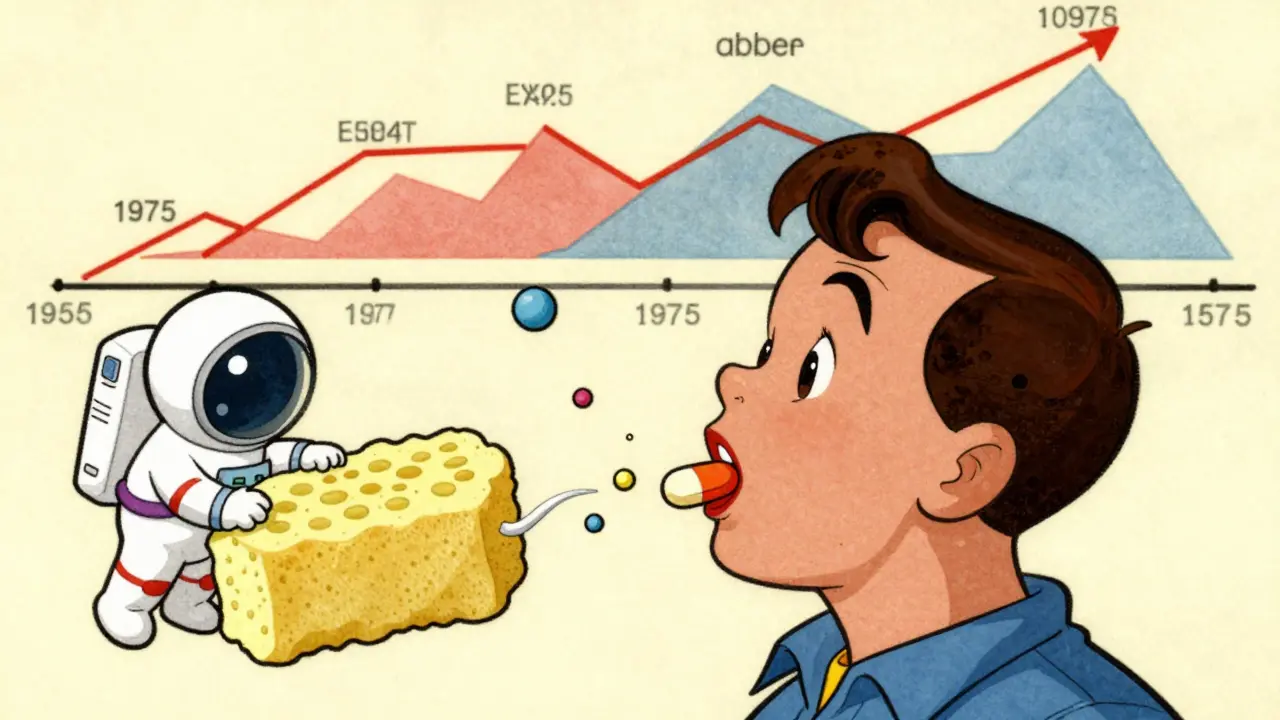
Since 1975, cases of esophageal adenocarcinoma have jumped 850%. Why? Because obesity has exploded. In the U.S., over 40% of adults are obese now-up from 15% in the 1970s. More fat means more pressure on the stomach. More pressure means more acid reflux. More reflux means more Barrett’s. More Barrett’s means more cancer.And yet, only 13% of high-risk people get the recommended screening. That’s a gap. A dangerous one. We have the tools. We know who’s at risk. We know what to do. But too many people are still flying blind.
What’s Next
New tools are coming. There’s a pill-sized sponge called Cytosponge that you swallow. It collects cells from your esophagus, and you don’t need an endoscope. In trials, it caught 80% of Barrett’s cases. That could change everything-especially for people who avoid endoscopy because they’re scared or can’t get access.Researchers are also looking at genetic markers. Some people have gene variants that make them more likely to develop Barrett’s from GERD. In the future, we might be able to test for those and personalize screening.
But right now, the best tool you have is awareness. Know your risk. Know the red flags. Don’t brush off heartburn as “just stress” or “eating too late.” If you’ve had it for five years or more, especially with other risk factors, get checked. Your esophagus can’t tell you it’s in trouble. You have to listen.
Can GERD cause esophageal cancer even if I take medication?
Yes. Medication like PPIs helps reduce acid and lowers your cancer risk by up to 70% if taken consistently for five years-but it doesn’t eliminate it. If you’ve had GERD for more than five years, especially with other risk factors, you still need endoscopic screening to check for Barrett’s esophagus. Medication controls symptoms, but it doesn’t reverse cellular changes that may have already happened.
Is esophageal cancer hereditary?
Not directly, but family history matters. If a close relative had esophageal cancer, your risk increases. This could be due to shared genetics, lifestyle, or diet. It doesn’t mean you’ll get it, but it does mean you should be screened earlier and more carefully, especially if you also have GERD.
Do I need a screening if I have GERD but no symptoms?
Yes-if you’ve had GERD for five or more years and you’re a man over 50 with obesity, smoking history, or family history. Some people have silent reflux-acid damage without heartburn. That’s why guidelines focus on duration and risk factors, not just symptoms. If you’ve been on acid meds for years, you’re still at risk.
Can I reverse Barrett’s esophagus?
In some cases, yes. Lifestyle changes-losing weight, quitting smoking, taking PPIs, and avoiding triggers-can cause Barrett’s to regress. Endoscopic treatments like radiofrequency ablation can remove abnormal tissue and reduce cancer risk by over 90%. But this only works if caught early. Once cancer develops, reversal isn’t possible.
What’s the survival rate if caught early?
If esophageal cancer is found before it spreads (localized stage), the 5-year survival rate is 50% to 60%. That’s more than double the overall rate of 21%. But 75% of cases are diagnosed too late. Early detection through screening for high-risk people is the only way to improve survival.






Bradford Beardall
January 10, 2026 AT 04:45Man, I had no idea GERD could turn into cancer like this. I’ve been on PPIs for 7 years and thought I was fine. Just got my doc to schedule an endoscopy after reading this. Feels weird to say it, but I’m kinda glad I stumbled on this post.
McCarthy Halverson
January 11, 2026 AT 07:53Barrett’s is real. Got diagnosed last year. PPIs help but don’t fix the damage. Endoscopy every 2 years now. Don’t wait like I did.
Jake Kelly
January 11, 2026 AT 08:37This is the kind of info that should be on every doctor’s waiting room wall. Thanks for laying it out so clearly. I’m sharing this with my dad-he’s 62, smokes, and has had heartburn since he was 45.
Ritwik Bose
January 11, 2026 AT 15:27Thank you for this deeply informative post 🙏. In India, many still think acid reflux is just 'spicy food problem'. I will share this with my family and community. Awareness saves lives. 🌏❤️
Paul Bear
January 13, 2026 AT 09:20Let’s be precise: the 0.2%-0.5% annual progression rate to adenocarcinoma is only applicable to confirmed Barrett’s esophagus with intestinal metaplasia. Many clinicians overdiagnose Barrett’s based on visual cues alone-histology is gold standard. Also, PPIs reduce risk but don’t eliminate metaplastic transformation. If you’re asymptomatic and have no dysplasia, surveillance intervals can be extended beyond 3 years. Don’t panic. Just get the right test.
Jaqueline santos bau
January 13, 2026 AT 12:29I’ve been ignoring my reflux for 8 years because I thought it was ‘just stress’… and now I’m terrified. I’m 52, overweight, and I smoked for 20 years. I just cried reading this. I’m calling my doctor tomorrow. Please tell me I’m not too late.
Kunal Majumder
January 15, 2026 AT 01:15Bro, I’m 48, Indian, had GERD since 30, never thought it was serious. Just drank buttermilk and thought I was good. After reading this, I booked an endoscopy. Best thing I did this year. You’re not alone.
Aurora Memo
January 15, 2026 AT 07:04To everyone panicking in the comments: you’re not alone, and you’re not doomed. Early detection works. I had low-grade dysplasia found during screening-ablated it, now I’m monitored yearly. I’m alive because I listened. You can be too.
chandra tan
January 15, 2026 AT 14:36My uncle died of this in 2020. No symptoms until he couldn’t swallow water. We didn’t know. This post saved me. I quit smoking. Lost 15 lbs. Got screened. All clear so far. Stay vigilant, folks.
Dwayne Dickson
January 16, 2026 AT 09:31So let me get this straight… we’ve got a preventable cancer epidemic fueled by obesity, corporate food systems, and a healthcare system that only intervenes after the damage is done. And yet we’re still telling people to ‘just take a pill’ and ‘watch their diet’ like it’s a personal failing? The system is broken. Screening should be universal for anyone over 50 with >5 years of reflux. Not a privilege. A right.
anthony martinez
January 18, 2026 AT 02:04Yeah sure, PPIs reduce risk by 70%. But did you also know that long-term PPI use increases risk of C. diff, kidney disease, and B12 deficiency? So now you’re trading one problem for three others. Maybe the real solution isn’t suppressing acid-it’s fixing the root cause. Just saying.
Christine Milne
January 18, 2026 AT 15:26This is all nonsense. Esophageal cancer is a rare disease. You’re scaring people with statistics that don’t apply to them. In my country, we don’t overtest for everything. If you don’t have symptoms, don’t get an endoscopy. It’s expensive, invasive, and unnecessary. Stop fearmongering.