After giving birth, many new parents expect joy. But for postpartum depression, the reality can be exhaustion, numbness, guilt, and a crushing sense of failure-even when everything looks perfect on the outside. It’s not just being tired. It’s not just the ‘baby blues.’ It’s a real medical condition that affects about 1 in 7 new mothers and 1 in 10 new fathers. And while hormones play a big part, they’re not the whole story.
What’s Really Going On With Your Hormones?
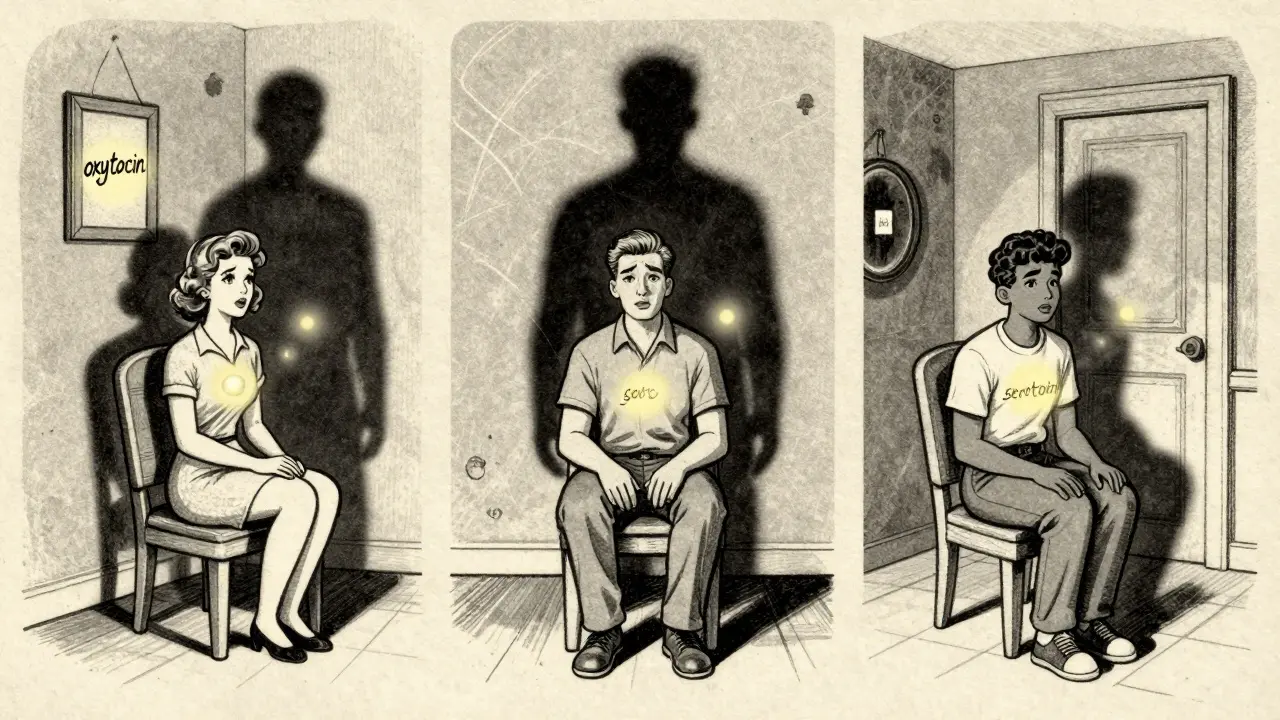
During pregnancy, your body floods with estrogen and progesterone-levels rise up to ten times higher than normal. Then, within two to three days after delivery, they drop back to pre-pregnancy levels. That’s not a slow fade. It’s a crash. Your brain, which has adapted to those high levels over nine months, suddenly has to readjust. This sharp shift can throw off mood-regulating chemicals like serotonin and dopamine.
One key player is allopregnanolone, a metabolite of progesterone. It helps calm the nervous system. When it drops after birth, that calming effect disappears. That’s why some women feel wired, irritable, or on edge-even if they’ve never had anxiety before. Studies show lower levels of oxytocin during the third trimester also link to higher depression risk. Oxytocin, often called the ‘love hormone,’ spikes during breastfeeding and skin-to-skin contact. Less of it? More stress, more sadness.
But here’s the twist: not every woman with a hormonal crash gets postpartum depression. And some women with PPD have hormone levels that look completely normal. That’s because hormones don’t act alone. They interact with your genetics, your stress levels, your sleep, your support system, and even your gut bacteria. One 2019 study in JAMA Psychiatry found no consistent difference in estrogen or progesterone levels between women with and without PPD. So while hormones create a vulnerable state, they don’t cause it by themselves.
It’s Not Just Moms-It’s All Parents
Postpartum depression doesn’t care if you gave birth or adopted. It doesn’t care if you’re cisgender, transgender, or nonbinary. Research shows transgender and nonbinary parents experience PPD at similar rates as cisgender women. Adoptive parents aren’t immune either-6 to 8% develop symptoms. And dads? About 1 in 10 experience postnatal depression, especially if they’re sleep-deprived, financially stressed, or have a partner who’s struggling.
Demographics matter too. CDC data from 2021 shows American Indian and Alaska Native mothers face PPD rates of over 20%, compared to 14% among non-Hispanic white mothers. That gap isn’t about biology. It’s about access to care, systemic stress, and lack of community support.
Other big risk factors? A history of depression-even if it was years ago. A traumatic birth. A baby with health problems. Isolation. A partner who’s emotionally unavailable. Financial pressure. Lack of sleep. These aren’t just ‘bad luck.’ They’re real, measurable triggers that stack up with hormonal shifts to push someone over the edge.
What Treatments Actually Work?
There’s no one-size-fits-all fix, but multiple proven options exist. First-line treatment? Therapy. Cognitive behavioral therapy (CBT) has a 52% response rate in studies-nearly double the improvement seen in control groups. Talking to a trained therapist helps you reframe negative thoughts, build coping skills, and process the emotional weight of new parenthood.
Medication is another powerful tool. SSRIs like sertraline are often the first choice because they’re safe during breastfeeding. Studies show very low levels pass into breast milk, and no major side effects have been found in nursing babies. Other options include escitalopram and fluoxetine, but sertraline has the strongest safety track record. It usually takes 4 to 6 weeks to feel the full effect, so patience is key.
For severe cases, newer options are changing the game. In 2019, the FDA approved brexanolone (Zulresso), an IV infusion of allopregnanolone. It works fast-sometimes in hours. But you have to stay in a hospital for 60 hours with constant monitoring because it can cause extreme drowsiness or fainting. In 2023, zuranolone (Zurzuvae) became the first oral version of the same drug. You take it for two weeks at home. It’s a major step forward: effective, faster than SSRIs, and no hospital stay.
For those who don’t respond to meds or therapy, transcranial magnetic stimulation (TMS) is showing promise. A 2020 study found 68% of women with treatment-resistant PPD improved after six weeks of daily TMS sessions. It’s non-invasive, doesn’t require anesthesia, and has few side effects beyond mild scalp discomfort.
What Doesn’t Work (And Why)
Some people think popping a few estrogen pills will fix it. There’s some evidence it can help-back in 2001, a small study found 82% of women with PPD improved after taking sublingual estrogen. But the risks? Blood clots, stroke, and disrupted milk supply. The FDA hasn’t approved hormonal treatments for PPD because the benefits don’t outweigh the dangers for most people.
And while rest, vitamins, or ‘just thinking positive’ sound nice, they won’t fix a clinical depression. PPD isn’t weakness. It’s not laziness. It’s a brain chemistry issue, often triggered by biology and stress. Telling someone to ‘snap out of it’ is like telling someone with a broken leg to walk it off.
Screening and Support Are Critical
Most cases go undiagnosed because no one asks. That’s why screening is so important. The Edinburgh Postnatal Depression Scale (EPDS) is used worldwide. It’s a simple 10-question quiz. A score of 10 or higher signals possible depression. Massachusetts was the first state to make screening mandatory in 2012. Now, more OB-GYNs and pediatricians are doing it.
But here’s the problem: 78% of OB-GYNs say they don’t feel trained to treat PPD. That’s why peer support matters. Postpartum Support International runs a warmline (1-800-944-4773) that fields about 25,000 calls a year. People who call say 87% found the support ‘helpful’ or ‘very helpful.’ Just knowing you’re not alone can be the first step toward healing.

What Should You Do If You’re Struggling?
If you’re feeling hopeless, overwhelmed, or disconnected from your baby-even for a few days-it’s time to reach out. Don’t wait for it to get worse. Talk to your doctor, midwife, or pediatrician. Ask for a referral to a therapist who specializes in perinatal mental health. If you’re breastfeeding, ask about medication safety. Sertraline is usually the safest bet.
If you’re in crisis-having thoughts of harming yourself or your baby-call 999 or go to the nearest emergency room. You are not a bad parent. You are not broken. You are sick, and you need help. That’s not weakness. That’s courage.
And if you’re supporting someone with PPD? Don’t say, ‘You’re lucky to have a baby.’ Don’t offer unsolicited advice. Just say, ‘I’m here.’ Bring food. Hold the baby while they nap. Listen without trying to fix it. Sometimes, that’s the most powerful treatment of all.
Looking Ahead
Research is moving fast. Scientists are now studying gut bacteria to see if certain microbes increase PPD risk. Others are looking at genetic markers to predict who’ll respond best to which treatment. The goal? Personalized care-knowing exactly which therapy or drug will work for you, before you start.
For now, the message is clear: postpartum depression is common, treatable, and nothing to be ashamed of. Hormones play a role, but they’re just one piece of a much bigger puzzle. With the right support, the right treatment, and the right timing, recovery isn’t just possible-it’s likely.






Niamh Trihy
January 29, 2026 AT 12:43I’ve been through PPD after my second kid, and honestly, the biggest help wasn’t meds or therapy-it was having someone just sit with me while I cried. No advice, no ‘you’re doing great,’ just presence. That’s what saved me. The hormonal crash is real, but isolation makes it ten times worse.
Also, if you’re breastfeeding and worried about SSRIs-sertraline is the gold standard. My lactation consultant gave me the study numbers, and it’s safer than most people think. Talk to your doctor, but don’t let fear stop you from getting help.
Jason Xin
January 30, 2026 AT 15:55Yeah, sure. Hormones are the villain. Next you’ll tell me my dog’s barking is caused by moon phases. Look, I’m a dad. I didn’t get pregnant. I didn’t have the estrogen crash. But I was the one holding the baby at 3 a.m. while my wife stared at the ceiling like a ghost. And nobody talks about how dads get treated like emotional janitors.
My wife got screened, got meds, got support. I got ‘maybe you should try yoga.’ Thanks, healthcare system. Real helpful.
Kathleen Riley
February 1, 2026 AT 06:40One must acknowledge the ontological dissonance inherent in the postpartum condition: the biological imperative to nurture, juxtaposed with the existential void precipitated by the abrupt cessation of gestational homeostasis. The hormonal precipice, while empirically measurable, is but a symptom of a deeper metaphysical rupture-the dissolution of the prepartum self into the uncharted territory of maternal identity.
It is not merely serotonin depletion, but the collapse of the Cartesian ego under the weight of intersubjective responsibility. To reduce this to pharmacological intervention is to mistake the map for the territory.
Beth Cooper
February 1, 2026 AT 09:56Okay but have you heard about the 2022 CDC whistleblower report? They buried the data showing that PPD is actually caused by 5G towers near maternity wards. The FDA approved Zulresso not because it works, but because they’re scared of the truth.
Also, all the ‘experts’ are in the pocket of Big Pharma. I know a mom who took vitamin D and magnesium and her PPD vanished in 72 hours. No hospital. No drugs. Just pure earth energy. They don’t want you to know this.
And why is everyone ignoring the fact that babies are now being born with microchips? Coincidence? I think not.
Donna Fleetwood
February 1, 2026 AT 21:20You are NOT alone. Seriously. I was in the darkest place after my son was born-I thought I was failing as a mom. But I reached out to a local group, and within two weeks I was laughing again. It’s not magic. It’s not weakness. It’s just biology + stress + no sleep + society telling you to ‘just be happy.’
Try TMS if meds don’t work. It’s weird but amazing. I did 6 weeks of it. No side effects, just quiet relief. And if you’re scared to ask for help? Text someone right now. Just say ‘I’m not okay.’ That’s enough. You don’t have to explain. You don’t have to earn it.
You’re doing better than you think. I promise.
Melissa Cogswell
February 3, 2026 AT 12:53Just wanted to add-gut health matters more than people think. One 2021 study showed that women with low microbial diversity in their gut had higher inflammation markers and were 3x more likely to develop PPD. Probiotics aren’t a cure, but they’re a legit supportive tool.
Also, if you’re on SSRIs and breastfeeding, check the LactMed database. It’s free, evidence-based, and way more reliable than random Reddit advice. Sertraline is still #1, but fluoxetine can build up over time. Small details matter.
Diana Dougan
February 4, 2026 AT 16:31So let me get this straight. You’re telling me the whole medical system is just now figuring out that hormones affect mood? Newsflash: I’ve been on birth control since I was 16 and I’ve been crying over spilled milk since 2017. This isn’t ‘postpartum depression,’ it’s ‘female biology is a glitch.’
And why are we still using the EPDS? That thing was designed in 1987. It asks if you’ve cried in the last week. So… am I depressed because I watched a sad dog video? I think not.
Also, ‘dad depression’? Please. Men don’t get depressed. They just get angry and start fixing things. Like the car. Or the Wi-Fi. Or the baby’s crib. That’s not depression. That’s patriarchy.
Bobbi Van Riet
February 5, 2026 AT 02:53I’m a therapist who specializes in perinatal mental health, and I’ve seen so many people get misdiagnosed because their doctor didn’t ask the right questions. Like, ‘Do you feel like you’re a burden to your partner?’ or ‘Do you feel guilty for not loving your baby the way you thought you would?’ Those are the real red flags.
Also, people don’t realize that PPD can show up 6 months after birth. I had a client who was fine at 2 weeks, then completely shut down at 7 months. No one thought to check because ‘she’s not a newborn anymore.’ But the brain doesn’t reset on a calendar.
And if you’re in a rural area and can’t find a specialist? Try telehealth. A lot of therapists now offer sliding scale rates. You don’t need to suffer in silence. Seriously. I’ve had clients who cried in their first session because no one had ever asked them how they felt. Just asking is a gift.
Holly Robin
February 6, 2026 AT 09:22THEY’RE LYING TO YOU. EVERY SINGLE ONE OF THEM. The ‘hormone crash’ is a distraction. The real cause? The government is injecting synthetic oxytocin into the water supply to make mothers more compliant. You think your baby’s crying is normal? It’s a signal. A biological alarm. They don’t want you to wake up.
And why is Zulresso only available in hospitals? Because they don’t want you to heal at home. They want you dependent. They want you on meds forever. Look at the pharma stock prices since 2019. Coincidence? I think not.
Also, the ‘1 in 7’ stat? That’s a lie. It’s actually 1 in 3. They lowered the number so they wouldn’t have to fund real care. I’ve seen the leaked emails. I have screenshots. I’ll post them if you want. You’re being gaslit by the system.
Shubham Dixit
February 7, 2026 AT 19:03Listen, in India we don’t have this problem because we have family. Grandmother, aunties, cousins-they all help. No one expects a woman to do it alone. No therapy. No pills. Just food, touch, and endless chai. We don’t need fancy drugs. We need community.
And you Americans think you’re so advanced with your TMS and Zulresso? Pathetic. You’ve lost the village. You’ve turned motherhood into a clinical trial. In my village, if a woman cries, we hold her. We don’t give her a questionnaire and send her to a lab.
Stop overcomplicating. You don’t need a PhD to be a mother. You need a warm lap, a hot meal, and someone who doesn’t ask if you’re ‘feeling okay’-they just sit with you.
Also, why is everyone ignoring the fact that Western medicine has killed 300 million women through unnecessary C-sections? That’s the real epidemic. Not depression. Over-medicalization.