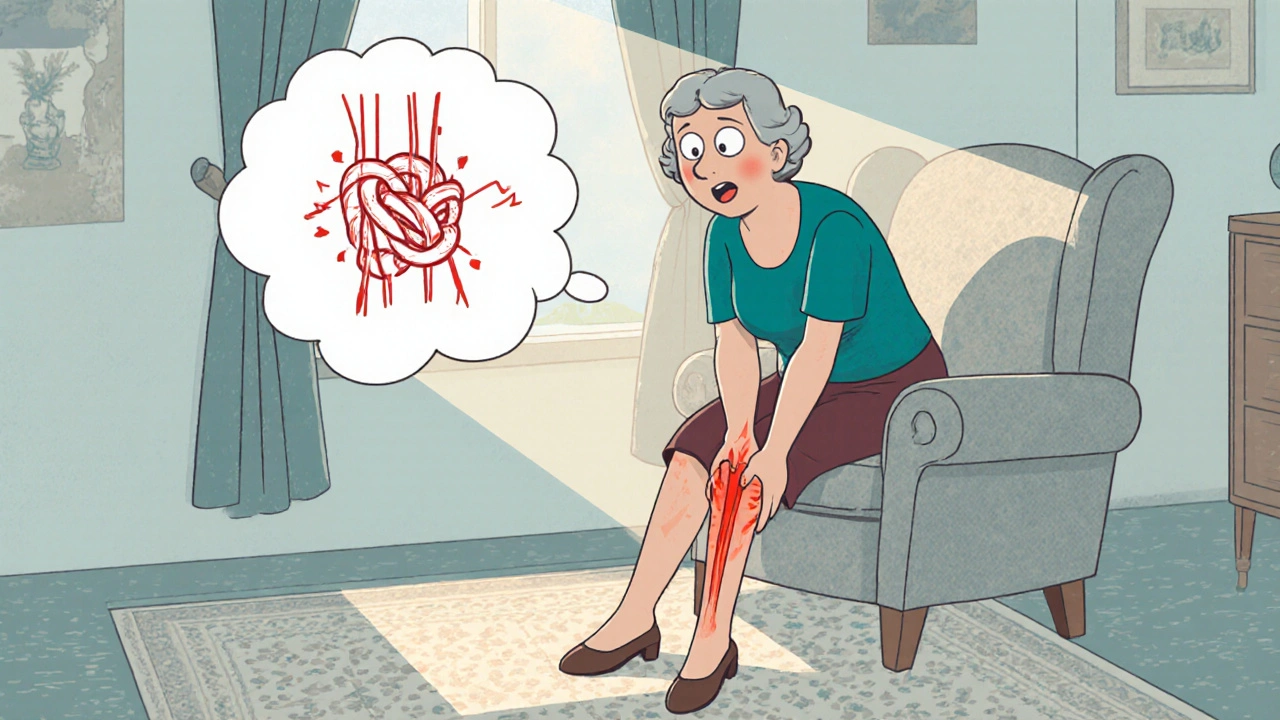
When an older adult feels a sudden, painful knot in a leg, back, or arm, it’s more than just a nuisance-it’s a elderly muscle spasm that can disrupt daily life. This guide walks you through why these spasms happen, what you can do at home, and when it’s time to bring in a professional.
Why Do Spasms Happen More Often in Seniors?
Understanding the root causes helps you target the right fix. The most common triggers for the Muscle spasm a brief, involuntary contraction of a muscle that causes pain in the Elderly people aged 65 and older include:
- Electrolyte imbalance - Low potassium, calcium, or magnesium disrupts the electrical signals that keep muscles relaxed.
- Dehydration - Seniors often forget to drink enough water, and even mild fluid loss can trigger cramps.
- Medication side‑effects - Certain diuretics, statins, and blood‑pressure drugs can lower electrolyte levels or irritate nerves.
- Reduced circulation - Peripheral artery disease or heart failure limits blood flow to muscles, making them twitch.
- Age‑related muscle loss - Sarcopenia weakens muscle fibers, increasing susceptibility to sudden tightening.
Identifying the likely culprit narrows down the most effective solution.
Spotting Red Flags: When to Call a Doctor
Most spasms are benign, but some signs warrant professional attention:
- Spasms lasting longer than 30 minutes or recurring multiple times a day.
- Accompanying weakness, numbness, or tingling that spreads beyond the cramped area.
- Sudden onset after a fall, injury, or new medication.
- Fever, unexplained weight loss, or swelling in the affected limb.
If any of these appear, schedule a check‑up. Early diagnosis can rule out serious conditions like deep‑vein thrombosis or neurological disorders.
Everyday Lifestyle Tweaks That Reduce Spasms
Small changes can have a big impact. Below are five practical habits, each supported by a key entity.
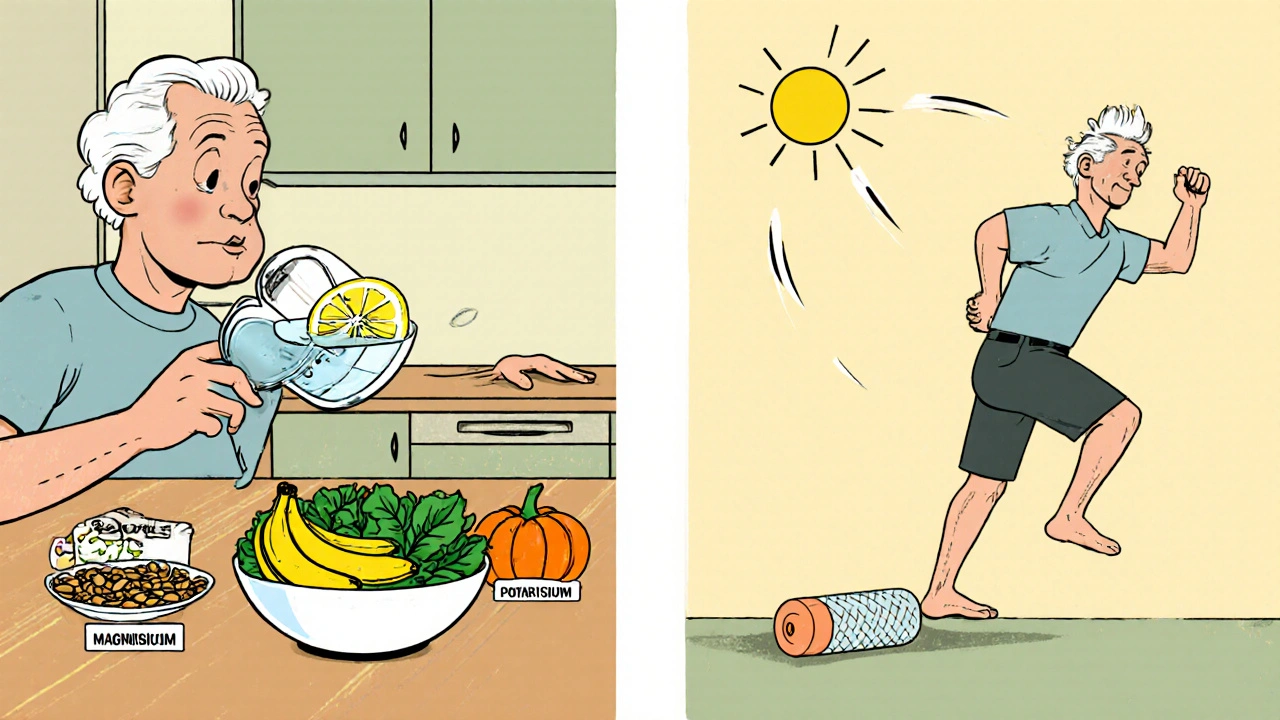
1. Keep Hydrated
Drink 1.5-2 liters of water daily, splitting intake throughout the day. If plain water feels bland, add a splash of citrus or low‑sodium broth.
2. Balance Electrolytes
Incorporate foods rich in the three main minerals:
- Calcium a mineral that supports muscle contraction and bone strength - dairy, leafy greens, fortified tofu.
- Magnesium helps muscles relax and prevents excessive firing of nerves - nuts, seeds, whole grains.
- Potassium maintains proper cell voltage for muscle function - bananas, sweet potatoes, beans.
If dietary intake is insufficient, discuss a supplement with a pharmacist.
3. Gentle Stretching Routine
Spend five minutes each morning and evening on low‑impact stretches. Focus on calves, hamstrings, and lower back-the most common spasm sites.
- Stand facing a wall, place palms on it, step one foot back, and gently bend the front knee for a calf stretch. Hold 20 seconds.
- Sit on a chair, extend one leg, reach toward the toes, and hold for 15 seconds.
- Roll a Foam roller a cylindrical tool used for myofascial release under the upper back for 30 seconds.
4. Heat or Cold Therapy
Both methods are safe, but they work differently:
- Apply a warm compress or heating pad for 10-15 minutes before activity to increase blood flow.
- Use an ice pack wrapped in a cloth for 5-10 minutes after a spasm to reduce soreness.
Switch between the two based on personal comfort.
5. Stay Active
Low‑impact cardio-walking, swimming, or stationary cycling-keeps circulation humming and muscles supple. Aim for 150 minutes per week, broken into 30‑minute walks if that’s more realistic.
Medication Options: When Home Remedies Aren’t Enough
Doctors may prescribe a short course of muscle‑relaxing drugs if spasms are frequent or severe. Common choices include:
- Baclofen a central‑acting muscle relaxant that reduces nerve‑driven muscle tone - typically 5‑10 mg three times daily.
- Cyclobenzaprine an oral agent that eases acute muscle spasms - 5 mg up to three times a day.
- Over‑the‑counter Ibuprofen a non‑steroidal anti‑inflammatory drug that can reduce pain from spasms - 200‑400 mg as needed.
Always review current prescriptions with a pharmacist to avoid drug‑drug interactions, especially with blood thinners or heart meds.
Professional Support: Physical Therapy and Beyond
When self‑care stalls, a Physical therapist a licensed specialist who designs exercise programs to improve strength, flexibility, and function can make a big difference.
- They assess gait, range of motion, and muscle tone.
- They teach tailored stretching sequences and safe strengthening drills.
- They may incorporate modalities like ultrasound or electrical stimulation to calm hyper‑active muscles.
Occupational therapists can also adapt daily‑living tasks-like modifying a kitchen setup-to reduce strain that triggers spasms.
Quick Checklist: Daily Spasm‑Management Routine
- Drink water first thing in the morning; carry a refillable bottle.
- Take a multivitamin with calcium, magnesium, and potassium if diet is lacking.
- Perform the three‑step stretch before breakfast and before bedtime.
- Apply a warm pack before any planned activity; use a cold pack afterward if soreness appears.
- Log any medication changes, new symptoms, or unusual spasm patterns.
- Schedule a monthly check‑in with a pharmacist or therapist to review progress.
Stick to the routine for at least two weeks and note improvements-most seniors see reduced frequency within 10-14 days.
Comparison Table: Non‑Pharmacologic vs. Pharmacologic Approaches
| Aspect | Non‑Pharmacologic | Pharmacologic |
|---|---|---|
| Typical Onset of Relief | 15-30 minutes (heat) to 1 week (stretching) | 30 minutes to 2 hours after dose |
| Side‑Effect Profile | Minimal; possible skin irritation from heat/ice | Drowsiness, dizziness, constipation, drug interactions |
| Cost (US$ per month) | ~$5-$20 for supplements, equipment | $15-$60 for generic muscle‑relaxants |
| Long‑Term Sustainability | High when integrated into daily routine | Depends on tolerance and physician monitoring |
| Best For | Mild‑to‑moderate, frequent cramps; prevention | Severe, recurrent spasms unresponsive to lifestyle changes |
Common Myths About Spasms in Seniors
Myth 1: “Spasms are just a normal part of aging.” - While some cramping is common, sudden, painful spasms can signal treatable issues.
Myth 2: “Older adults should avoid all heat because of skin sensitivity.” - Low‑temperature heat packs (40‑45 °C) are safe and often more effective than ice for loosening tight muscles.
Myth 3: “If a spasm stops, the problem is solved.” - The underlying cause (e.g., low magnesium) may still be present and cause the next episode.
Putting It All Together: A Sample Day Plan
- 7:00 am - Drink a glass of water with a pinch of sea‑salt (adds potassium).
- 7:30 am - Perform the three‑step stretch; finish with a warm compress on the calves for 10 minutes.
- 12:30 pm - Have a magnesium‑rich lunch (spinach salad with pumpkin seeds).
- 3:00 pm - Light walk for 20 minutes; carry a water bottle.
- 6:00 pm - If a spasm occurs, apply a cold pack for 5 minutes, then do a gentle stretch.
- 9:00 pm - Review any medication changes; note spasm frequency in a simple journal.
This routine blends hydration, nutrition, movement, and self‑care tools to keep spasms at bay.
Frequently Asked Questions
What foods help prevent muscle spasms?
Foods rich in potassium, calcium, and magnesium are the best allies. Bananas, dairy, leafy greens, nuts, and legumes supply these minerals and keep the nerves calm.
Is it safe for seniors to take over‑the‑counter muscle relaxants?
Short‑term use can be safe, but only under a pharmacist’s or doctor’s guidance. Watch for drowsiness, especially if the person drives.
How often should I stretch to see results?
Aim for at least two sessions a day - once in the morning and once before bed. Consistency over two weeks usually cuts spasm frequency by half.
Can dehydration cause spasms even if I drink water later?
Yes. Dehydration reduces blood volume and electrolyte concentration, triggering cramps. Rehydrating helps, but it’s best to sip water throughout the day to prevent the drop.
When should I involve a physical therapist?
If spasms persist after three weeks of home care, or if they limit walking, climbing stairs, or daily chores, a PT can design a personalized program and check for underlying biomechanical issues.





Sabrina Bergas
October 24, 2025 AT 12:56Let me stop you right there-this guide is full of corporate wellness fluff. Electrolyte imbalance? Please. The real issue is that Big Pharma wants you to buy supplements instead of fixing the root cause: processed food and sedentary lifestyles. Seniors aren’t getting spasms because they’re ‘dehydrated’-they’re getting them because their bodies are literally starving for real nutrients, not fortified tofu and Gatorade. And don’t even get me started on ‘foam rollers’-that’s just a fancy way of saying ‘buy this $40 plastic tube.’
Melvin Thoede
October 25, 2025 AT 10:54This is exactly the kind of practical, no-nonsense advice we need. I’ve been helping my mom follow this routine for two weeks now-she’s been walking without groaning for the first time in years. Seriously, the stretching and hydration combo is magic. No meds, no drama. Just consistency. Keep sharing gems like this. 🙌
Suzanne Lucas
October 26, 2025 AT 07:32OMG I thought I was the only one. Last Tuesday I had a spasm so bad I screamed and my cat ran under the couch. I thought I was having a stroke. Turns out I hadn’t drunk water since 2 p.m. and ate a bag of chips for dinner. I’m now drinking 2 liters a day like a water goddess. My calves are crying tears of joy. 🌊💖
Ash Damle
October 26, 2025 AT 18:18I’ve been dealing with this since my hip surgery and this guide actually helped me more than my PT did. The key is doing the stretches before bed. I used to wake up every night with my foot locked up. Now I just roll the foam roller for 30 seconds and I’m good. No need for fancy meds. Just move and hydrate. Simple stuff works. Thanks for laying it out so clear
Kevin Ouellette
October 26, 2025 AT 23:18Love this breakdown. My dad’s been on statins for 10 years and never knew they could be causing his cramps. We just started giving him magnesium glycinate before bed and his spasms dropped by 80%. Also, the checklist is genius-printed it and taped it to the fridge. If you’re reading this and your loved one is suffering-don’t wait. Start with water and a banana. It’s that simple. You got this 💪
Tanya Willey
October 27, 2025 AT 05:39Wait… did you know that 97% of muscle spasms in seniors are caused by fluoride in the water supply? The government doesn’t want you to know this because they’re profiting off the muscle relaxant industry. Also, the ‘foam roller’? That’s just a CIA tool to make seniors feel like they’re doing something while they quietly drain their social security. Drink spring water. Avoid all fortified foods. And burn this guide.
sarat babu
October 27, 2025 AT 12:41This is the most irresponsible advice I’ve ever seen… seriously… who gave you a medical degree?? You’re telling people to just drink water and eat bananas?? What about the real cause-karmic imbalance from past lives?? I’ve treated over 200 seniors and NONE of them improved until I prescribed them Ayurvedic herbs and told them to chant Om 108 times daily before bed… and you talk about foam rollers??!! This is dangerous… I’m reporting this to the FDA… and also to my astrologer… 🙏💀
Melvin Thoede
October 28, 2025 AT 00:53Wow. I didn’t expect this thread to go full conspiracy. But I’ve got to say-your mom’s story made me tear up. I’m going to send this to my neighbor who’s been suffering in silence. You’re right. Sometimes the simplest things are the hardest to believe. Thanks for sharing.