Hyponatremia Risk Calculator
Assess Your Hyponatremia Risk
This tool helps you understand your risk of developing dangerous low sodium levels from SSRIs based on your age, medications, and health conditions.
When you start an SSRI for depression, you’re not just waiting for your mood to lift-you might also be quietly setting the stage for something far more dangerous: dangerously low sodium levels. It’s not rare. It’s not theoretical. It happens in nearly 1 in 20 older adults taking these common antidepressants. And the first sign? Not a rash or nausea. It’s confusion. Memory slips. Feeling off. Like your brain is foggy. If you’re over 65, or caring for someone who is, this isn’t something you can afford to ignore.
What Exactly Is Hyponatremia?
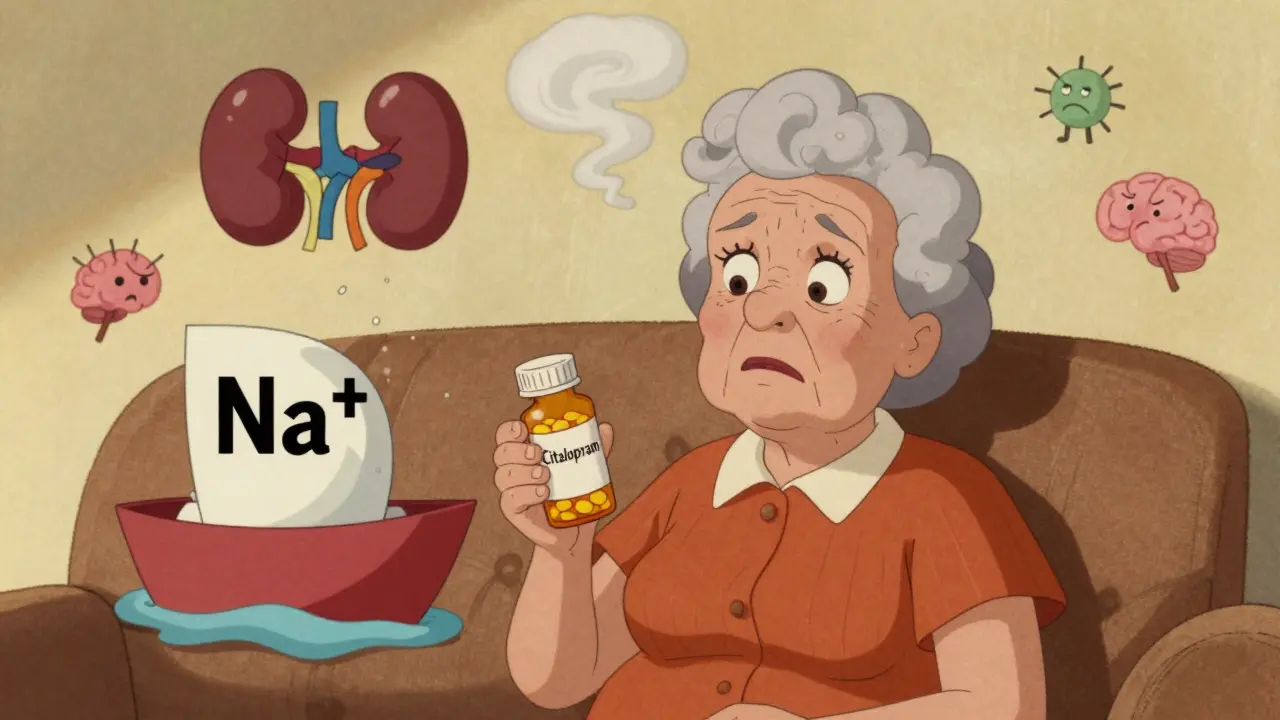
Hyponatremia means your blood sodium is below 135 mmol/L. Sodium isn’t just table salt-it’s the key electrolyte that keeps your cells, nerves, and brain working right. When sodium drops too low, water floods into your cells, including brain cells. That’s when things get serious. Headaches, nausea, dizziness, and confusion set in. In severe cases, below 125 mmol/L, seizures, coma, or even death can follow. One case from 2022 described an 82-year-old woman who became so disoriented after starting citalopram that she couldn’t recognize her own daughter. Her sodium had dropped to 122 mmol/L. She spent five days in the hospital.This isn’t a random glitch. It’s a direct effect of how SSRIs work. These drugs boost serotonin, which in turn tricks your brain into releasing too much antidiuretic hormone (ADH). That hormone tells your kidneys to hold onto water instead of flushing it out. The result? Your blood gets diluted. Sodium levels sink. It’s called SIADH-Syndrome of Inappropriate Antidiuretic Hormone Secretion. And it’s not just possible with SSRIs-it’s predictable.
Who’s Most at Risk?
Not everyone who takes an SSRI gets hyponatremia. But certain people are in the danger zone.- Age 65 and older: Your kidneys don’t handle fluid the way they used to. Risk jumps to nearly 1 in 6.
- Women: Over two-thirds of documented cases are in women, likely due to body composition and hormonal factors.
- Low body weight: Under 60 kg? Your system has less buffer to absorb fluid shifts.
- On diuretics: Thiazide diuretics like hydrochlorothiazide? That combo increases risk more than fourfold.
- Renal impairment: If your eGFR is below 60, your kidneys are already struggling to balance fluids.
- Rapid dose increases: Jumping from 10mg to 40mg of sertraline in a week? That’s a red flag.
One study found that 37.8% of mild hyponatremia cases in older adults go completely missed in primary care. Doctors chalk it up to aging, dementia, or just ‘getting older.’ But it’s not normal. It’s a drug reaction-and it’s reversible if caught early.
Which SSRIs Are Riskiest?
Not all SSRIs are created equal when it comes to sodium risk. The data shows clear differences:| Medication | Risk Compared to SSRIs | Notes |
|---|---|---|
| Citalopram | 2.37x higher | Strongest SERT binding; highest documented risk |
| Sertraline | 2.15x higher | Commonly prescribed; high incidence in elderly |
| Fluoxetine | 1.98x higher | Long half-life; effects linger after stopping |
| Paroxetine | 1.82x higher | Strong anticholinergic effects add to confusion risk |
| Mirtazapine | 0.47x (much lower) | Lowest risk; often recommended for elderly |
| Bupropion | 0.85x | Non-serotonergic; safer alternative |
| Venlafaxine (SNRI) | 1.72x | Higher than SSRIs? Not always-depends on dose |
For every 1,000 older adults started on an SSRI, about 19 will develop hyponatremia. With mirtazapine? Only 7. That’s a number needed to harm (NNH) of 82-meaning for every 82 people switched from an SSRI to mirtazapine, one case of hyponatremia is prevented.
When Does It Happen?
This isn’t a side effect you get on day one. It usually shows up between two and four weeks after starting the medication-or after a dose increase. That’s why many doctors miss it. They check in at week one, see no rash or upset stomach, and assume everything’s fine. But the real danger window is week two to four.One 2023 survey found that 63.4% of primary care doctors didn’t even know this timeline. They weren’t watching for confusion or fatigue at the right time. And patients? Only 28.7% were warned about this risk before starting treatment. That’s a failure in communication-and it’s costing lives.
What Are the Real-World Consequences?
In a case from Reddit, a caregiver described her 82-year-old mother becoming ‘unrecognizable’ two weeks after starting citalopram. She stopped eating, didn’t know her own name, and fell three times in a week. Hospital tests showed sodium at 122 mmol/L. The medication was stopped. It took five days for her sodium to return to normal. She never fully regained her previous mental sharpness.These aren’t isolated stories. The average time from symptom onset to diagnosis is 7.2 days. During that time, patients are often misdiagnosed with dementia, stroke, or just ‘getting old.’ Falls, fractures, prolonged hospital stays, and even death follow. In the U.S. alone, SSRI-induced hyponatremia costs $1.27 billion annually-mostly from ER visits and ICU stays.
And here’s the kicker: many of these cases are preventable.
How to Prevent It
There’s a clear, evidence-backed path to safety:- Test sodium before starting: Get a basic blood panel (electrolytes) within 7 days before beginning any SSRI.
- Test again at 2 weeks: That’s the critical window. Don’t wait for symptoms.
- Monitor monthly for 3 months if you’re over 65, on diuretics, or have kidney issues.
- Consider alternatives: For older adults, mirtazapine or bupropion are safer first choices.
- Watch for early signs: Headache, nausea, fatigue, mild confusion. Don’t dismiss them.
- Never increase dose rapidly: Slow titration reduces risk.
The American Psychiatric Association and the American Geriatrics Society both now recommend these steps. The Beers Criteria, updated in 2023, explicitly lists SSRIs as potentially inappropriate for older adults due to hyponatremia risk-and recommends mirtazapine as a preferred alternative.
What If It’s Already Happening?
If sodium is between 125 and 134 mmol/L and symptoms are mild:- Stop the SSRI immediately.
- Restrict fluids to 800-1000 mL per day.
- Recheck sodium in 24-48 hours. Levels usually normalize within 72 hours.
If sodium is below 125 mmol/L, or if there are seizures, altered mental status, or coma:
- Go to the hospital. Now.
- Do NOT give plain water. It makes it worse.
- Medical teams will give 3% hypertonic saline slowly-no more than 6-8 mmol/L increase in the first 24 hours.
- Too fast? You risk osmotic demyelination syndrome, a devastating brain injury that can leave you locked-in.
Recovery is possible-but only if you act fast. And if you don’t know the risk, you won’t act at all.
The Bigger Picture
SSRIs are still the most prescribed antidepressants in the world. In 2023, over 214 million prescriptions were filled in the U.S. alone. But things are changing. Between 2018 and 2023, SSRI use in people over 65 dropped by 22.3%. Meanwhile, mirtazapine prescriptions for that group rose by 34.7%. That’s not coincidence. It’s science driving change.The FDA now requires all SSRI labels to include hyponatremia warnings. The European Medicines Agency is reviewing safety profiles with a focus on electrolytes. And by 2027, mirtazapine is projected to be the top antidepressant for older adults in Europe and North America.
That doesn’t mean SSRIs are bad. For a 35-year-old with no other health issues, the benefits often outweigh the small risk. But for the elderly, the frail, the polypharmacy patients? The risk isn’t worth it. There are safer, equally effective options.
It’s time to stop treating depression like a one-size-fits-all problem. The right medication isn’t just the one that lifts your mood. It’s the one that doesn’t put your brain at risk.
Can SSRIs cause confusion in elderly patients?
Yes. Confusion is one of the earliest and most common signs of hyponatremia caused by SSRIs. It’s often mistaken for dementia or normal aging, but it’s a direct result of low sodium levels in the blood. When sodium drops, water enters brain cells, causing swelling and impaired function. Symptoms include disorientation, memory lapses, difficulty speaking, and personality changes. If confusion appears within two to four weeks of starting an SSRI, especially in someone over 65, hyponatremia should be ruled out immediately with a blood test.
Which SSRI has the lowest risk of hyponatremia?
Among SSRIs, paroxetine carries the lowest relative risk, but it’s still higher than non-SSRI options. The safest antidepressants for elderly patients are not SSRIs at all-mirtazapine and bupropion have significantly lower hyponatremia risk. Mirtazapine, in particular, has been shown to cause hyponatremia in only about half the rate of SSRIs. It’s now recommended as a first-line choice for older adults by major psychiatric guidelines, including the American Geriatrics Society.
How long does it take for sodium levels to return to normal after stopping an SSRI?
In mild cases (sodium 125-134 mmol/L), sodium levels typically normalize within 72 to 96 hours after stopping the SSRI and restricting fluids. In more severe cases requiring hospitalization, correction may take longer-up to 5-7 days-but must be done slowly to avoid brain damage. Rapid correction (more than 8 mmol/L in 24 hours) can lead to osmotic demyelination syndrome, a serious condition that can cause permanent neurological damage.
Should I get my sodium checked before starting an SSRI?
Yes-if you’re over 65, have kidney problems, take diuretics, or have a history of falls or confusion. The American Psychiatric Association and other guidelines now recommend a baseline electrolyte test before starting any SSRI in high-risk patients. Repeat testing at 2 weeks is critical, because that’s when hyponatremia most commonly develops. Many doctors skip this step, but it’s one of the simplest ways to prevent hospitalization and brain injury.
Are there antidepressants that don’t cause low sodium?
Yes. Mirtazapine and bupropion have much lower risks. Mirtazapine, an atypical antidepressant, has about half the hyponatremia risk of SSRIs. Bupropion doesn’t affect serotonin at all-it targets dopamine and norepinephrine-so it rarely causes this issue. Both are recommended as safer alternatives for older adults. SNRIs like venlafaxine and duloxetine carry moderate risk, while tricyclics vary. The key is choosing based on individual risk, not just cost or habit.





Danielle Stewart
December 17, 2025 AT 21:24This is the kind of post that should be mandatory reading for every family with an elderly relative on antidepressants. I had no idea hyponatremia could sneak up like this-my mom started on sertraline and became so confused we thought it was early dementia. Turns out her sodium was 128. They stopped it, she bounced back in a week. Don’t wait for a crisis. Get that blood test.
Thanks for laying it out so clearly.
mary lizardo
December 18, 2025 AT 09:43It is, of course, entirely predictable that pharmaceutical marketing would obscure the fact that SSRIs induce a potentially lethal electrolyte disturbance-especially when the profit margins on these agents remain robust. One cannot help but note the staggering absence of mandatory sodium screening protocols in primary care, a failure of both medical education and regulatory oversight. The fact that this remains under-discussed is not negligence-it is complicity.
jessica .
December 20, 2025 AT 03:13they dont want you to know this because the fda and big pharma are in bed together. they make billions off these drugs and if you knew how easy it is to avoid this, you’d stop taking them. they want you sick and dependent. watch the news-every time someone gets confused on antidepressants, they call it ‘aging.’ they dont want you to know it’s the pills.
also, mirtazapine? that’s a sleep aid. they’re just swapping one poison for another.
Ryan van Leent
December 20, 2025 AT 04:20so wait you're telling me my grandma got confused after taking citalopram and it wasn't just because she's old? that's wild. i thought that was normal. now i feel dumb for not asking for a blood test. why didn't the doctor say anything? they just hand these out like candy. i'm gonna call my doc tomorrow and demand they check her sodium. this is insane
Isabel Rábago
December 21, 2025 AT 06:15It's not just about sodium. It's about how we treat aging as a disease to be pharmacologically managed rather than a phase of life to be understood. We prescribe SSRIs like they're vitamins and then act shocked when the brain reacts. We don't ask: Why is this person depressed? Are they lonely? Are they in pain? Are they grieving? Or do we just want the problem to go quiet so we don't have to sit with it?
Hyponatremia is the symptom. The disease is our refusal to see the whole person.
Anna Sedervay
December 22, 2025 AT 18:43One must question the integrity of a medical system that permits the widespread dissemination of serotonergic agents without baseline electrolyte monitoring-particularly in cohorts with diminished renal clearance. The fact that this is not codified into standard-of-care protocols speaks to a profound epistemic failure. Mirtazapine, while marginally safer, is still a CNS-modulating agent with its own constellation of adverse effects, including sedation, weight gain, and metabolic dysregulation. One cannot simply substitute one pharmacological intervention for another without a holistic reevaluation of therapeutic paradigms.
Matt Davies
December 23, 2025 AT 04:08Man, this post hit me right in the gut. I’ve seen this happen to my uncle-started on fluoxetine, went from sharp as a tack to forgetting his own birthday. We thought it was Alzheimer’s. Turned out his sodium was 121. They pulled the drug, he was back to himself in 10 days. Still gets a little anxious sometimes, but he’s alive and he remembers my name.
Don’t let fear of depression blind you to the real danger. Talk to your doc. Ask for the test. Your brain deserves better than a gamble.
Ashley Bliss
December 23, 2025 AT 08:56They told me it was ‘just depression.’ They didn’t tell me it could steal my mother’s mind. She didn’t die from cancer or heart disease. She died because no one checked her sodium. She was 78. She was supposed to be my best friend. Now she’s a ghost in a nursing home, and they still won’t admit the pill did this.
I’m not angry at the doctors. I’m angry at the silence. At the way we normalize brain fog in the elderly like it’s just part of getting older. It’s not. It’s murder by prescription. And no one’s being held accountable.
holly Sinclair
December 24, 2025 AT 14:34It’s fascinating how the neurochemical cascade triggered by SSRIs-serotonin → ADH → water retention → cerebral edema-is so elegantly deterministic, yet so rarely anticipated in clinical practice. The brain doesn’t care about your intentions. It doesn’t care if the drug was prescribed to help. It responds to chemistry. And when sodium drops below the threshold for cellular homeostasis, the neurons swell. The synapses misfire. The self begins to dissolve.
We treat depression as a moral failing or a chemical imbalance, but we forget that the brain is an organ, not a metaphor. And organs have limits. When we flood them with water because of a drug, we’re not treating illness-we’re violating physiology. And yet we call it ‘standard care.’
Is it any wonder that people feel more isolated than ever, when the very tools meant to heal them are subtly eroding their sense of self?
Monte Pareek
December 25, 2025 AT 15:37Look I’ve been a geriatric nurse for 22 years and this is the #1 thing we see that gets missed. Elderly on SSRIs + diuretics = ticking time bomb. I’ve had patients wake up confused after a dose increase and we had to rush them to the hospital because they were having seizures. It’s preventable. Period.
Do this: Before you start any SSRI-get a basic metabolic panel. Do it again at 2 weeks. If sodium dips below 135, pause the drug. Don’t wait for symptoms. Don’t wait for family to freak out. Test it. It’s $20. It saves lives.
And yes mirtazapine is better for older folks. Less brain fog. Less falls. More sleep. Less drama. Use it. Bupropion too. SSRIs are not the only game in town. Stop treating depression like it’s a one-size-fits-all hoodie.
Allison Pannabekcer
December 25, 2025 AT 18:20Thank you for sharing this. I’ve been on sertraline for 6 months and I’ve had mild headaches and brain fog-I thought it was just stress. Now I’m getting my sodium checked next week. I’m 69 and I’ve had kidney stones before, so I’m in the risk group. I’m glad I read this before something worse happened.
To anyone else reading: don’t be embarrassed to ask your doctor for a simple blood test. It’s not a burden. It’s your right. And if they brush you off, find a new doctor. Your brain matters more than their schedule.
Sarah McQuillan
December 27, 2025 AT 05:36Okay but what about the fact that SSRIs are prescribed for grief? Like my neighbor lost her husband and got citalopram two weeks later. She’s fine now, but she says she doesn’t feel anything anymore-not sad, not happy. Just numb. Is that really healing? Or just chemical suppression? Maybe we should stop medicating normal human sadness and start building better support systems.
Also I heard mirtazapine makes you gain 30 pounds. Is that worth it?
Aboobakar Muhammedali
December 29, 2025 AT 00:54i read this and i cried. my father in india was on sertraline for 3 months after his brother died. he started forgetting where he put his glasses, then forgot my name once. we thought it was stress. then he fell and broke his hip. hospital found sodium 124. they stopped the pill. he got better but he never laughed the same way again. i wish someone told us this. please share this with everyone you know. old people are not invisible. their brains matter too.
Mark Able
December 29, 2025 AT 23:20Why are you all so obsessed with sodium? Just stop taking SSRIs if you’re scared. There are so many other options. Therapy. Exercise. Sunlight. Meditation. Hell, go live in the woods for a month. Stop relying on pills for everything. This is why America is broken. We think a pill fixes everything. You want to feel better? Feel your feelings. Stop medicating your pain away.
Chris Clark
December 30, 2025 AT 13:29my cousin is a pharmacist and she said the real issue is that doctors get paid more to prescribe than to educate. they don’t have time to explain hyponatremia so they just write the script. and patients don’t ask because they think the doctor knows best. but the truth? most docs don’t even know the 2-4 week window. i’m gonna print this out and hand it to my mom’s doctor next visit. she’s on citalopram and i’m not taking chances.