CLL Autoimmune Complication Prevalence Calculator
This tool provides data from clinical studies on the prevalence of autoimmune complications in Chronic Lymphocytic Leukemia patients. Click on a complication to see detailed information.
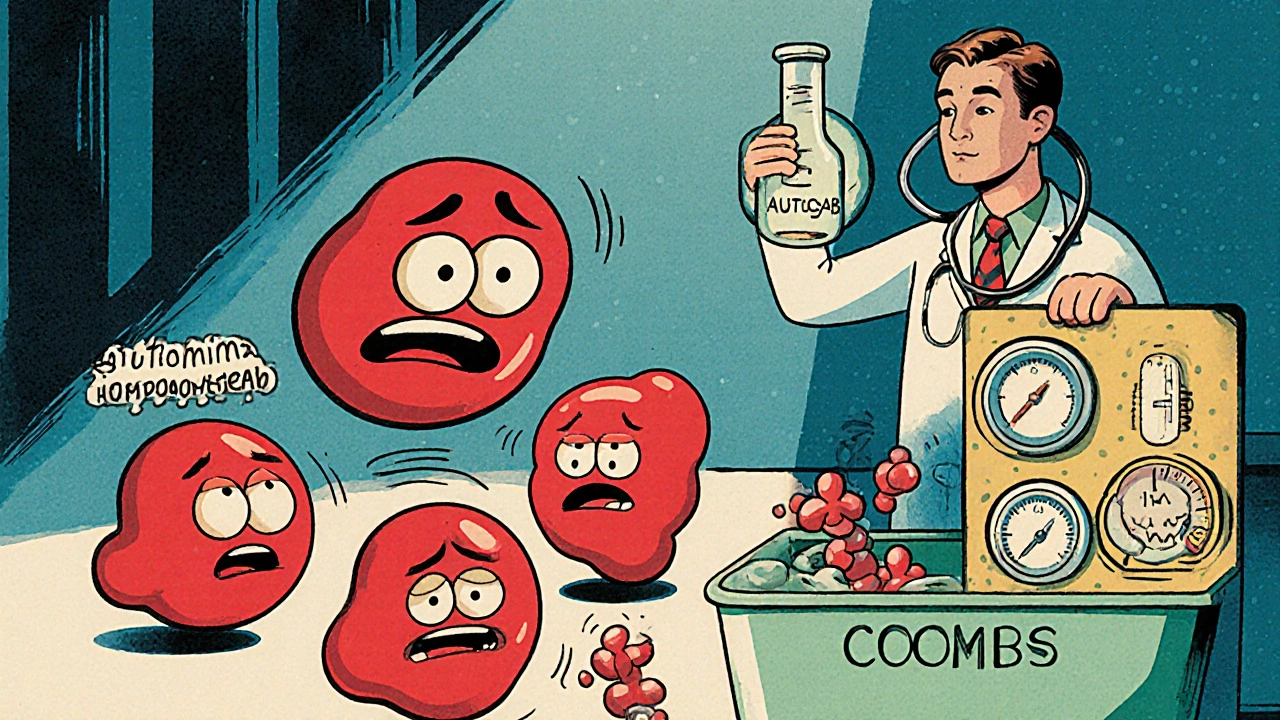
Autoimmune Hemolytic Anemia (AIHA)
Prevalence: 10-20% of CLL patients develop AIHA.
Key Diagnostic Test: Direct Coombs test.
AIHA occurs when the immune system attacks red blood cells, leading to anemia. It's one of the most common autoimmune complications in CLL, often requiring prompt treatment with steroids or rituximab.
Ever wondered why people with Chronic Lymphocytic Leukemia often develop conditions like anemia or low platelet counts? The answer lies in a tangled web of immune dysregulation, genetics, and treatment side‑effects. This article breaks down the science, points out the most common autoimmune complications, and shows how doctors keep the balance under control.
Key Takeaways
- About 20‑30% of CLL patients develop an autoimmune disorder, most frequently autoimmune hemolytic anemia (AIHA) or immune thrombocytopenia (ITP).
- Faulty B‑cell receptor (BCR) signaling and abnormal CD5+ B‑cells are the main culprits behind auto‑reactivity.
- Regular monitoring with flow cytometry and direct Coombs testing catches problems early.
- Treatment strategies combine CLL‑directed drugs (e.g., ibrutinib) with immunosuppressants like steroids or rituximab.
- Emerging therapies targeting the complement system and IL‑10 pathways hold promise for safer long‑term control.
Chronic Lymphocytic Leukemia is a slow‑growing cancer of mature B‑lymphocytes that typically appears in adults over 60. These malignant cells express the surface marker CD5, which is unusual for normal B‑cells and gives the disease its classic "CD5+ B‑cell" profile. Over time, the clonal expansion crowds out healthy blood cells, leading to infections, anemia, and enlarged lymph nodes.
Autoimmune diseases refer to conditions where the immune system mistakenly attacks the body’s own tissues. In the context of CLL, the most relevant ones are autoimmune hemolytic anemia (AIHA), immune thrombocytopenia (ITP), and less frequently, neutropenia or vasculitis.
Why Autoimmunity Is So Common in CLL
The link isn’t a coincidence. CLL cells retain the ability to produce antibodies, but they do so in a dysregulated way. Two molecular players stand out:
- B‑cell receptor signaling becomes chronic and hyper‑active, lowering the threshold for self‑reactive antibodies.
- CD5+ B‑cells are prone to escape normal tolerance checkpoints, allowing autoreactive clones to survive.
Meanwhile, the surrounding immune environment shifts. T‑cell dysfunction, reduced regulatory T‑cell (Treg) numbers, and an excess of cytokine IL‑10 create a permissive milieu for auto‑antibody production.
Common Autoimmune Complications in CLL
| Condition | Typical Prevalence | Key Diagnostic Test |
|---|---|---|
| Autoimmune hemolytic anemia (AIHA) | 10‑20% | Direct Coombs test |
| Immune thrombocytopenia (ITP) | 5‑10% | Platelet count + peripheral smear |
| Autoimmune neutropenia | 1‑3% | ANC < 1.5 × 10⁹/L with anti‑neutrophil antibodies |
| Vasculitis (small‑vessel) | ~1% | Skin biopsy, ANCA testing |
How Doctors Detect Autoimmune Activity
Early detection saves lives. The standard work‑up includes:
- Complete blood count (CBC) to spot anemia or low platelets.
- Direct antiglobulin (Coombs) test for AIHA.
- Peripheral blood smear to look for spherocytes or platelet clumping.
- Flow cytometry (Flow cytometry) to confirm the CLL immunophenotype (CD5+, CD19+, CD20dim).
- Serum complement levels - low C3/C4 can hint at complement‑mediated hemolysis.
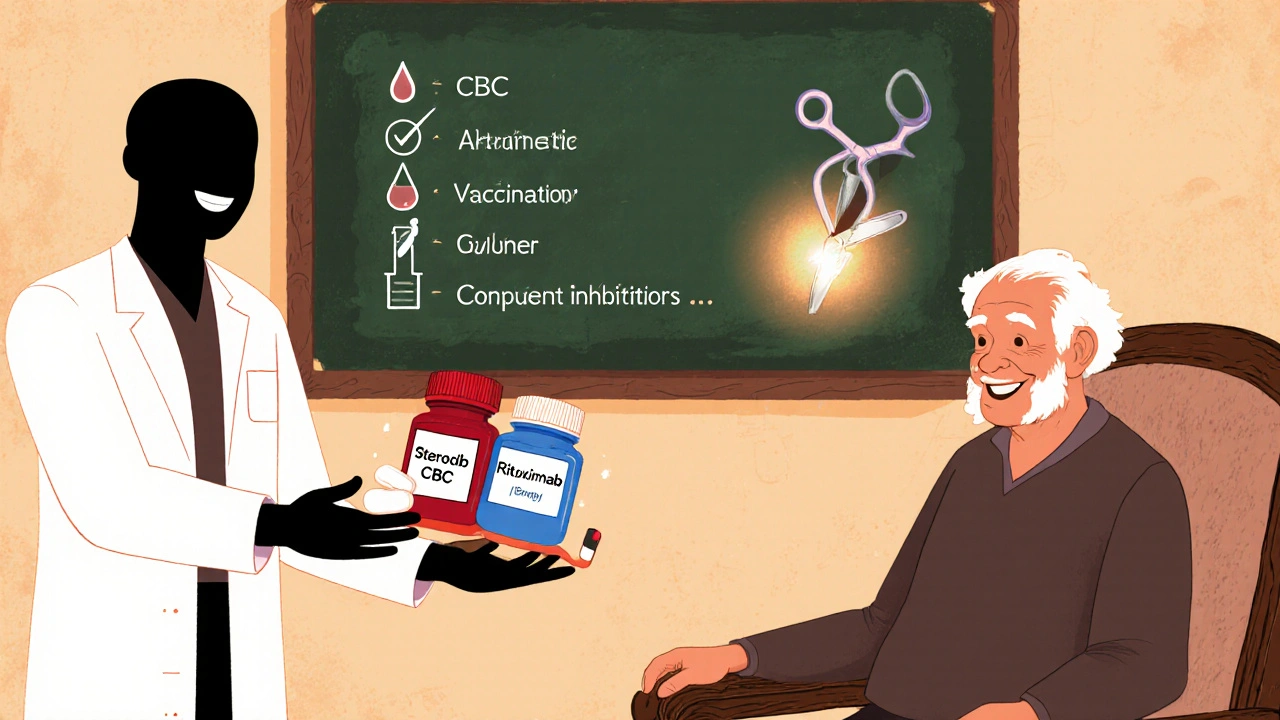
Managing the Double Threat
Treatment has two tracks: controlling the leukemia and quelling the autoimmune reaction.
- First‑line for AIHA/ITP: High‑dose corticosteroids (prednisone 1 mg/kg) often bring rapid remission.
- Steroid‑sparing agents: Rituximab (anti‑CD20) depletes both malignant and autoreactive B‑cells; it’s especially useful when steroids fail.
- Targeted CLL drugs: Ibrutinib (BTK inhibitor) not only shrinks the leukemic clone but also reduces auto‑antibody production in many patients.
- Complement inhibitors: Emerging agents like eculizumab are being tested for refractory AIHA cases.
- IL‑10 modulation: Early‑phase trials of anti‑IL‑10 antibodies aim to restore normal T‑cell balance.
When autoimmune complications dominate, clinicians may temporarily pause CLL‑directed therapy and focus on immune suppression, then restart once the counts stabilize.
Special Considerations
Some patients develop Richter transformation, where CLL converts into an aggressive lymphoma. Autoimmune phenomena can mask this progression, so any sudden worsening of cytopenias warrants a repeat biopsy.
Age matters, too. Older adults have reduced marrow reserve, making them more vulnerable to treatment‑related cytopenias. Dose adjustments and close monitoring are essential.
Future Directions
Research is homing in on the complement cascade and the role of regulatory cytokines. A 2024 multicenter study showed that adding a C1s inhibitor to standard steroid therapy lowered relapse rates of AIHA from 40% to 22% over 12 months.
Gene‑editing approaches (CRISPR‑Cas9) targeting the BCR signaling pathway are still pre‑clinical, but they hold the promise of eliminating the root cause of auto‑reactivity without broad immunosuppression.
Take‑Home Checklist for Patients and Caregivers
- Report any new fatigue, jaundice, or easy bruising immediately.
- Keep a copy of recent CBC results handy for every oncology visit.
- Ask your doctor about vaccination schedules - live vaccines are usually avoided after certain CLL therapies.
- Know the signs of steroid side effects (high blood sugar, mood changes) and discuss taper plans early.
- Stay informed about clinical trials targeting the complement system or IL‑10 pathways.
Frequently Asked Questions
Why does CLL increase the risk of autoimmune hemolytic anemia?
CLL cells produce abnormal antibodies that can bind to red‑blood‑cell antigens. Combined with a weakened immune‑regulatory network, these antibodies trigger red‑cell destruction, showing up as AIHA.
Can I take the flu vaccine if I have CLL?
Yes, the inactivated flu shot is recommended for most CLL patients. Live attenuated vaccines should be avoided, especially when you’re on BTK inhibitors or high‑dose steroids.
What is the role of rituximab in treating autoimmune complications?
Rituximab depletes CD20‑positive B‑cells, which includes both the malignant CLL clone and the autoreactive B‑cells that produce harmful antibodies. It’s often used when steroids alone are insufficient.
How often should I have blood tests to monitor autoimmunity?
During active treatment, a CBC every 2‑4 weeks is typical. Once stable, every 3‑6 months is adequate unless new symptoms appear.
Are there lifestyle changes that can lower my autoimmunity risk?
Maintaining a balanced diet, staying active, and avoiding smoking help overall immune health. However, specific lifestyle tweaks have not been proven to prevent CLL‑related autoimmunity.





Kevin Hylant
October 22, 2025 AT 13:20CLL's B‑cell dysregulation directly fuels auto‑antibody production, so monitoring Coombs and platelet counts is non‑negotiable. Early steroid intervention can keep AIHA in check.
Holly Green
October 22, 2025 AT 14:10It's essential that clinicians prioritize patient safety over experimental hype. Stick to proven steroids and rituximab before chasing new drugs.
Craig E
October 22, 2025 AT 15:16The interplay between chronic B‑cell receptor signaling and defective immune tolerance creates a perfect storm for autoimmunity in CLL.
When the signaling cascade remains perpetually active, even low‑affinity self‑reactive clones escape deletion.
These rogue B‑cells secrete antibodies that recognize red‑cell antigens, precipitating hemolysis.
Concurrently, regulatory T‑cells dwindle, removing a critical brake on immune activation.
The cytokine milieu, rich in IL‑10, further skews the balance toward antibody production.
Clinicians therefore rely on serial complete blood counts to catch trends before they spiral.
A sudden drop in hemoglobin or platelets should prompt a direct Coombs test without delay.
Flow cytometry not only confirms the CD5+ phenotype but can also quantify the proportion of clonally expanded B‑cells.
Targeted agents such as ibrutinib have demonstrated dual benefits: reducing leukemic burden and dampening auto‑antibody output.
Nevertheless, resistance mechanisms can emerge, necessitating adjunctive immunosuppression.
High‑dose prednisone remains the first‑line rapid response, yet its side‑effect profile demands careful tapering.
Rituximab offers a steroid‑sparing alternative by depleting CD20‑positive cells, both malignant and autoreactive.
For refractory cases, complement inhibitors like eculizumab are being explored with promising early data.
Patient education is paramount; individuals should report fatigue, jaundice, or bruising at the first hint.
Vaccination strategies must be individualized, avoiding live formulations during intensive immunosuppression.
Ultimately, a multidisciplinary approach that monitors laboratory parameters, adjusts therapy, and anticipates complications yields the best outcomes.
Oliver Johnson
October 22, 2025 AT 16:23Sure, but focusing on B‑cell signaling ignores the fact that many patients never develop autoimmunity despite similar signaling patterns, so genetics must dominate.
We should be careful not to attribute every cytopenia to the same mechanism.
Taylor Haven
October 22, 2025 AT 17:30The pharmaceutical lobby has been quietly steering research toward flashy complement inhibitors while keeping the cheap, effective steroids on the back burner.
Behind closed doors they fund trials that promise billions in revenue, yet the data on long‑term safety remain buried.
Meanwhile, insurance companies push patients into high‑cost BTK inhibitors without fully disclosing the modest impact on auto‑immune complications.
It's no coincidence that the most vocal proponents of eculizumab have ties to the same conglomerates that market rituximab.
Regulators are increasingly dependent on industry‑sponsored advisory panels, eroding unbiased oversight.
Patients are left to navigate a maze of jargon while the true cost of chronic immunosuppression-infectious doom, metabolic chaos-is downplayed.
Even academic conferences feature sponsored sessions that frame the narrative around novelty rather than necessity.
Data transparency is often limited to press releases, obscuring adverse event rates that could alter clinical guidelines.
This hidden agenda fuels an environment where experimental therapies are rushed to market before robust real‑world evidence is gathered.
Doctors, pressured by quotas and pharmaceutical reps, may unconsciously favor the newest drug over tried‑and‑true protocols.
Ultimately, the patient community must demand open data, independent review, and a focus on holistic care rather than profit‑driven hype.
Only then can we restore a balance that truly serves those battling CLL and its autoimmune shadow.
Sireesh Kumar
October 22, 2025 AT 18:36I get the frustration, but from my own experience the steroids really saved my sister when she hit a severe hemolytic crisis.
We tried a trial drug once and ended up hospitalized, so I still trust the tried-and-true regimen.
Ritik Chaurasia
October 22, 2025 AT 19:43In many Indian hospitals we see similar patterns, yet cultural dietary habits can influence baseline inflammation and perhaps modulate auto‑immune risk.
Jonathan Harmeling
October 22, 2025 AT 20:50While it's admirable to highlight cultural nuances, we mustn't excuse suboptimal treatment with folklore; evidence‑based therapy remains the cornerstone, regardless of cuisine.
Vandermolen Willis
October 22, 2025 AT 21:56Great summary, really helped me understand what to watch for! 😊
Steven Young
October 22, 2025 AT 23:03Honestly the whole system feels rigged the way pharma pushes pricey drugs while ignoring cheap steroids it’s like a circus of profit and patients suffer from side effects that could be managed with simple monitoring and timely intervention.
Kelly Brammer
October 23, 2025 AT 00:10Patients deserve transparent communication about risks.