When your heart valve doesn’t open or close right, your whole body feels it. You might not notice at first-just a little tired after walking up stairs, or short of breath when you bend over to tie your shoes. But if one of your four heart valves is narrowed (stenosis) or leaking (regurgitation), that’s not normal. It’s a serious condition that gets worse over time. Left untreated, severe valve disease can cut your life expectancy in half. The good news? Today’s treatments can restore your energy, your breathing, and your life-often with just a small incision or even no cut at all.
What Happens When Heart Valves Fail
Your heart has four valves: aortic, mitral, tricuspid, and pulmonary. They’re like one-way doors that keep blood flowing in the right direction. When they work, blood moves smoothly from chamber to chamber and out to your body. When they fail, two things go wrong: either the valve gets stiff and won’t open fully (stenosis), or it won’t close tight and lets blood leak backward (regurgitation).Aortic stenosis is the most common serious valve problem in older adults. About 2% of people over 65 have it. The valve leaflets become calcified-like rust on a hinge-and can’t open wide enough. Your left ventricle has to pump harder to push blood through the narrow opening. Over time, that muscle thickens, weakens, and can’t keep up.
Mitral regurgitation is more common than you might think. It happens when the mitral valve doesn’t seal shut, so blood flows back into the left atrium every time your heart contracts. In mild cases, you might feel fine. But when it’s severe, your heart can’t pump enough blood forward. You get tired fast, your lungs fill with fluid, and your body doesn’t get the oxygen it needs.
Not all valve problems are the same. Aortic stenosis patients often report chest pain, dizziness, or fainting. Mitral regurgitation usually shows up as fatigue and shortness of breath during activity. The symptoms are different because each valve handles a different part of the blood flow. But the end result is the same: your heart is overworked, and your body is under-supplied.
Stenosis vs. Regurgitation: Key Differences
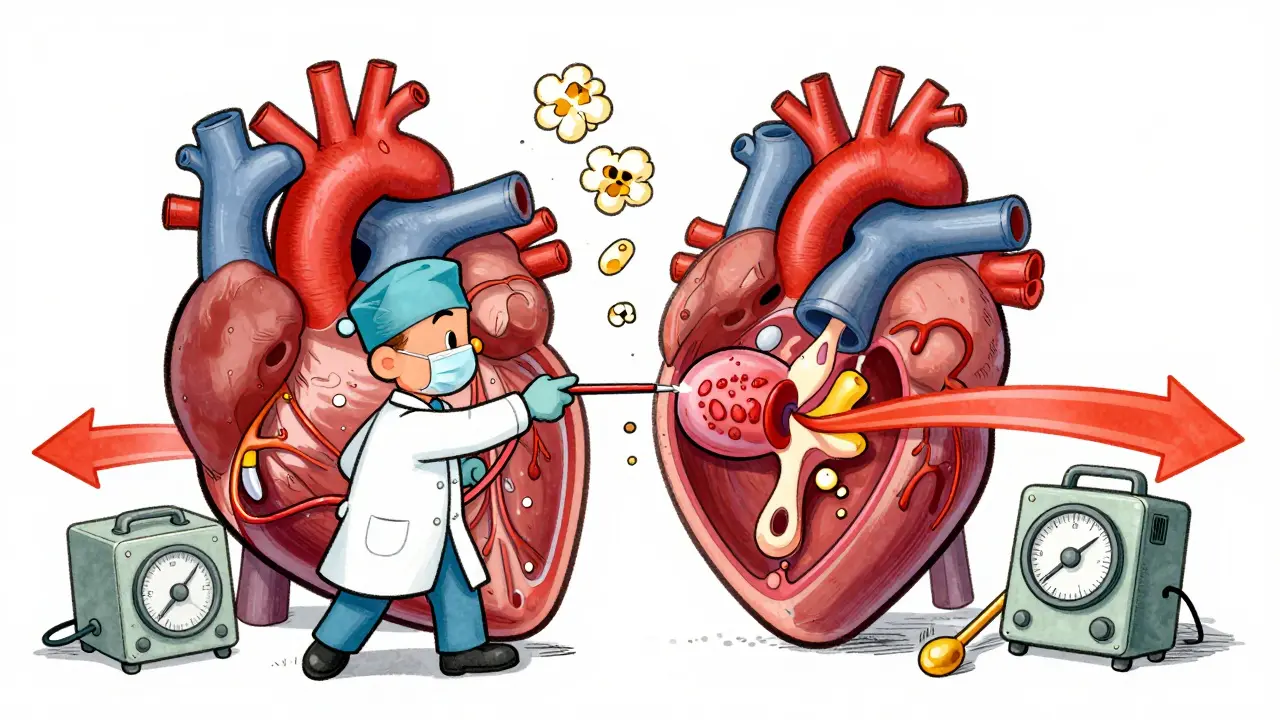
Stenosis and regurgitation sound similar, but they’re opposite problems with different consequences.
Stenosis is a pressure problem. The valve is too tight. Blood can’t flow out fast enough. The heart muscle thickens to compensate. Severe aortic stenosis is defined by a valve area smaller than 1.0 cm², a pressure gradient over 40 mmHg, and blood flow speed over 4.0 m/s. If your valve is that narrow, your heart is fighting a losing battle.
Regurgitation is a volume problem. The valve is leaky. Blood flows backward, so your heart has to pump extra to make up for what’s lost. In mitral regurgitation, the left ventricle gets stretched out. It doesn’t get stronger-it just gets bigger. That’s why many people with regurgitation feel fine for years, until suddenly they can’t catch their breath.
Here’s what sets them apart in real life:
- Aortic stenosis: 54% of patients have chest pain, 33% faint, 48% develop heart failure.
- Aortic regurgitation: 71% feel short of breath during activity, 29% notice their heart racing.
- Mitral stenosis: 68% struggle to lie flat without gasping (orthopnea).
- Mitral regurgitation: 79% report constant fatigue before symptoms become obvious.
These numbers aren’t random-they come from large patient studies. They show why timing matters. Waiting too long to treat stenosis can be deadly. Waiting too long to treat regurgitation can permanently damage your heart muscle.
What Causes Valve Problems?
Not all valve disease is the same. The cause changes depending on your age, location, and medical history.
In older adults, especially over 70, the most common cause of aortic stenosis is simple aging. Calcium builds up on the valve leaflets over decades. About 70% of cases are from this slow, silent process. But in younger people-under 70-about half of aortic stenosis cases come from a birth defect: a bicuspid aortic valve. Instead of three leaflets, it has two. That valve wears out faster. Many people don’t know they have it until their 50s or 60s, when symptoms start.
Mitral stenosis is different. In wealthy countries, it’s rare. But globally, 80% of cases are from rheumatic fever, a complication of untreated strep throat. It’s still common in parts of Africa, Asia, and Latin America. Rheumatic fever scars the valve, making it stiff and narrow. This is why heart valve disease is still a major issue in low-income countries.
Regurgitation can come from several places. Mitral regurgitation might be caused by a torn chordae tendineae (the cords that hold the valve in place), or from heart enlargement due to high blood pressure or coronary disease. In these cases, the valve itself is fine-it’s just being pulled apart by a stretched heart.
Surgical Options: From Open Heart to Tiny Catheters
For decades, open-heart surgery was the only option. A large incision down the chest, stopping the heart, connecting to a heart-lung machine. It worked-but recovery took months. Today, you have choices.
Surgical Valve Replacement (SAVR) is still the gold standard for many. A damaged valve is removed and replaced with a mechanical valve or a biological one made from animal tissue. Mechanical valves last forever but require lifelong blood thinners. Biological valves don’t need blood thinners long-term but wear out in 15-20 years. For younger patients, this means a second surgery later in life.
Transcatheter Aortic Valve Replacement (TAVR) changed everything. Instead of opening the chest, a catheter is threaded through an artery in the leg or chest. The new valve is compressed into a tiny tube, pushed to the heart, and expanded inside the old valve. No sternotomy. No heart stoppage. Hospital stay: 2-4 days. Recovery: weeks, not months.
TAVR is now the first choice for patients over 75 and for those with high surgical risk. The PARTNER 3 trial showed TAVR had 12.6% lower mortality than surgery at five years in low-risk patients. In 2023, 65% of aortic valve replacements in the U.S. for patients over 75 were done with TAVR. That’s up from just 12% in 2011.
For mitral regurgitation, you have options too. If the valve is damaged from disease (primary regurgitation), surgery to repair or replace it gives 90% survival at 10 years. But if it’s caused by heart failure (functional regurgitation), a device called MitraClip can be inserted through a vein in the leg. It clips the leaflets together to reduce the leak. The COAPT trial showed it cut death rates by 32% compared to medicine alone.
Even tricuspid valve repair is now possible with new devices like the Evoque system, approved by the FDA in March 2023. What was once considered untreatable is now fixable without open surgery.
When to Act-and When to Wait
One of the biggest mistakes doctors see is waiting too long. In aortic stenosis, once symptoms appear, 50% of patients die within two years without treatment. That’s why guidelines say: don’t wait for symptoms. If your valve is severely narrowed-even if you feel fine-it’s time to talk to a valve team.
But with regurgitation, it’s the opposite. If your valve leaks a little and your heart is still strong, you don’t need surgery. Pushing forward too early can expose you to unnecessary risks. Doctors monitor you with echocardiograms every 6-12 months. They look for signs your heart is starting to stretch or weaken. That’s when you act.
Dr. Catherine Otto, a leading expert, says: “Waiting for symptoms in aortic stenosis reduces 2-year survival to 50%.” But Dr. Robert Bonow warns: “Early intervention for mild regurgitation may subject patients to unnecessary surgical risks.”
It’s not about being aggressive. It’s about being precise. Your valve team-cardiologist, cardiac surgeon, imaging specialist-will weigh your age, symptoms, heart function, and overall health. They’ll use CT scans, echocardiograms, and stress tests to decide when the risk of doing nothing outweighs the risk of surgery.

What Recovery Really Looks Like
People imagine recovery from valve surgery as a quick fix. It’s not. It’s a journey.
After TAVR, most patients report feeling better in 30 days. Energy returns. Walking becomes easier. One patient on Reddit said: “After my MitraClip, I went from struggling to walk to the mailbox to hiking 3 miles daily within two months.”
But open-heart surgery? That’s harder. Sternotomy-the cut down the breastbone-takes weeks to heal. One patient on Inspire.com wrote: “The hardest part was the pain. I couldn’t lift my grandchildren for eight weeks.”
Anticoagulation is another reality. If you get a mechanical valve, you’ll need blood thinners like warfarin for life. You’ll need regular blood tests to check your INR. Too high, you risk bleeding. Too low, you risk clots. For mitral valves, the target is INR 2.5-3.5. For aortic, it’s 2.0-3.0. It’s a big commitment.
Bioprosthetic valves don’t need lifelong blood thinners, but they wear out. About 21% show signs of deterioration by 15 years. Newer tissue valves are designed to last longer-some may last 25+ years. But we’re still waiting for long-term data.
Why Many Patients Are Misdiagnosed
One of the most shocking facts? 28% of patients in a 2022 survey said they were dismissed by doctors until their symptoms became severe.
Why? Because valve disease is sneaky. It doesn’t show up on routine EKGs. It doesn’t raise your cholesterol or blood pressure. It doesn’t make you cough or fever. It just makes you tired. And tiredness is easy to blame on aging, stress, or being out of shape.
But if you’re over 65, have a heart murmur, or notice new fatigue, shortness of breath, or dizziness-get an echocardiogram. It’s quick. It’s painless. It’s the only way to know what’s really going on inside your heart.
Valve disease isn’t rare. It affects 13% of people over 75. Yet most people don’t know it exists. The more we talk about it, the fewer people will be left waiting until it’s too late.
What’s Next for Valve Treatment
The future is minimally invasive. By 2030, the American Heart Association predicts 80% of valve procedures will be done with catheters, not open surgery.
New devices are coming fast. The Cardioband system lets doctors shrink the mitral valve ring without cutting the chest. The Harpoon system lets surgeons repair the valve from inside the heart-no open incision needed. Both are in late-stage trials and could be approved by 2025.
Researchers are even working on valves made from lab-grown tissue. These could last longer, don’t need blood thinners, and might even grow with the patient-something no current valve can do.
But the biggest change isn’t the technology. It’s the mindset. Valve disease is no longer a death sentence. It’s a treatable condition. And the window to act? It’s wider than ever.
What are the early signs of heart valve disease?
Early signs are often mistaken for aging. You might feel unusually tired after light activity, get short of breath climbing stairs, or notice your heart racing without cause. Swelling in the ankles or feet, dizziness, or chest discomfort during exertion are also red flags. If you’re over 65 and have any of these, an echocardiogram is the only way to confirm valve disease.
Is TAVR better than open-heart surgery?
For patients over 75 or those with high surgical risk, TAVR is clearly better-it has lower mortality, faster recovery, and fewer complications. For younger, healthier patients under 65, surgical replacement still has longer durability data. But for patients aged 60-80, recent trials show TAVR is just as safe and effective as surgery. The choice depends on age, health, and valve anatomy-not just preference.
Can you live a normal life after valve replacement?
Yes-most people do. After recovery, many return to walking, gardening, traveling, and even playing with grandchildren. The key is following up with your cardiologist, taking medications as prescribed, and avoiding infections (like dental work without antibiotics). With modern valves and care, life expectancy after successful replacement is close to normal.
Do I need blood thinners after valve surgery?
It depends on the valve. Mechanical valves require lifelong blood thinners like warfarin. Biological valves usually need them only for 3-6 months after surgery. If you have atrial fibrillation or a history of clots, you may need them longer. Your doctor will monitor your INR levels and adjust your dose based on your valve type and overall risk.
How do I know if I need surgery or just monitoring?
You need a full valve assessment by a multidisciplinary team. They’ll look at your symptoms, echo results, heart function, and overall health. For aortic stenosis, surgery is recommended if the valve area is under 1.0 cm², even without symptoms. For regurgitation, surgery is advised when the heart starts to enlarge or pump weakly-before symptoms appear. Don’t wait for the worst symptoms. Get evaluated early.





Jonny Moran
December 16, 2025 AT 08:52It's not 'just aging' - it's your heart screaming for help.
jeremy carroll
December 17, 2025 AT 19:18Natalie Koeber
December 17, 2025 AT 23:01Daniel Thompson
December 19, 2025 AT 17:38Tim Bartik
December 21, 2025 AT 13:28Sarthak Jain
December 22, 2025 AT 23:11Edward Stevens
December 23, 2025 AT 19:45Alexis Wright
December 24, 2025 AT 01:51And don’t get me started on the cost. One TAVR valve = 30k. Insurance pushes it because they don’t want to pay for 20 years of home care. You’re not getting a miracle. You’re getting a profit margin.
Thomas Anderson
December 24, 2025 AT 23:31Daniel Wevik
December 25, 2025 AT 07:21Rulich Pretorius
December 25, 2025 AT 18:53Wade Mercer
December 27, 2025 AT 18:15Rich Robertson
December 29, 2025 AT 17:26Sinéad Griffin
December 31, 2025 AT 07:28