Driving While on Medication: Risks, Rules, and Safe Choices
When you’re on driving while on medication, the act of operating a vehicle while taking drugs that can impair cognitive or physical function. Also known as medication-impaired driving, it’s not just about alcohol or illegal drugs—it’s often prescription painkillers, sleep aids, or even allergy pills that catch people off guard. You might feel fine, but your reaction time could be 30% slower. Your vision might be blurry. Your brain might be foggy. And you won’t even know it until it’s too late.
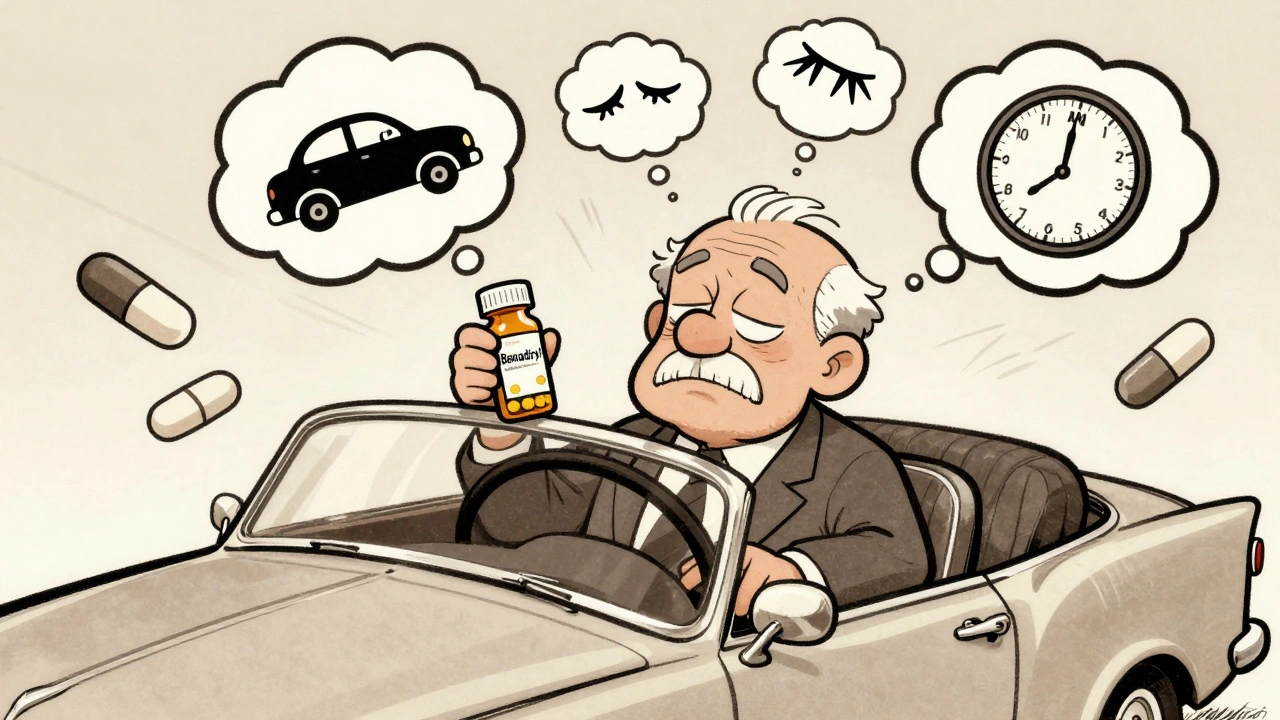
Sedating medications, drugs that cause drowsiness, slowed reflexes, or reduced alertness are the biggest hidden risk. First-generation antihistamines like diphenhydramine (Benadryl) are in cold meds, sleep aids, and even some pain relievers. They’re everywhere. And they’re not safe behind the wheel. Combine them with opioids, benzodiazepines, or even just a glass of wine, and you’re looking at CNS depressant interactions, when multiple drugs slow down the central nervous system, increasing drowsiness, dizziness, and risk of respiratory failure. The CDC says over 10% of drivers involved in crashes tested positive for impairing medications—not alcohol. That’s not a small number. That’s a silent epidemic.
It’s not just about feeling sleepy. Some meds make you dizzy when you stand up. Others blur your vision or make it hard to focus on moving objects. If you’re taking anything for chronic pain, anxiety, insomnia, allergies, or even an overactive bladder, check the label. Look for words like "may cause drowsiness," "use caution when operating machinery," or "avoid alcohol." If you see those, don’t assume you’re fine. You’re not. Even if you’ve taken it for years. Your body doesn’t build up a tolerance to impairment—it just gets used to feeling weird.
What about second-generation antihistamines like loratadine or fexofenadine? Those are safer. They don’t cross the blood-brain barrier as much, so they don’t make you drowsy. Same with non-sedating pain relievers like acetaminophen instead of opioids. But even those aren’t risk-free if you’re mixing them with other drugs. And if you’ve got liver disease or are over 65, your body processes meds slower. That means even a normal dose can build up and hit you like a truck.
You don’t need to stop taking your meds. You just need to know which ones are dangerous behind the wheel. Talk to your pharmacist. Ask your doctor: "Is this safe to drive on?" Don’t wait until you get pulled over or crash before you ask. The law doesn’t care if you didn’t mean to. If your meds impaired you, you’re legally responsible. And the consequences aren’t just fines—they’re lives.
Below, you’ll find real, practical advice from people who’ve been there. How to spot the warning signs. What to swap out. When to wait. And how to talk to your doctor without sounding paranoid. This isn’t fear-mongering. It’s about staying alive—and keeping others safe too.
Medications and Driving: How Common Drugs Impair Your Ability to Drive and What It Means Legally
- 11 Comments
- Dec, 1 2025
Many common medications impair driving more than people realize-even those prescribed by doctors. Learn which drugs are dangerous behind the wheel, the legal risks, and how to stay safe.
