Medication Driving Risk Calculator
This tool estimates your risk of impaired driving based on medications you're taking, age, and other factors. The information is based on medical research about how common drugs affect driving ability.
Note: This is for informational purposes only. Always consult your doctor or pharmacist before driving while taking any medication.
Driving While on Medication Isn’t Just Risky-It’s Often Illegal
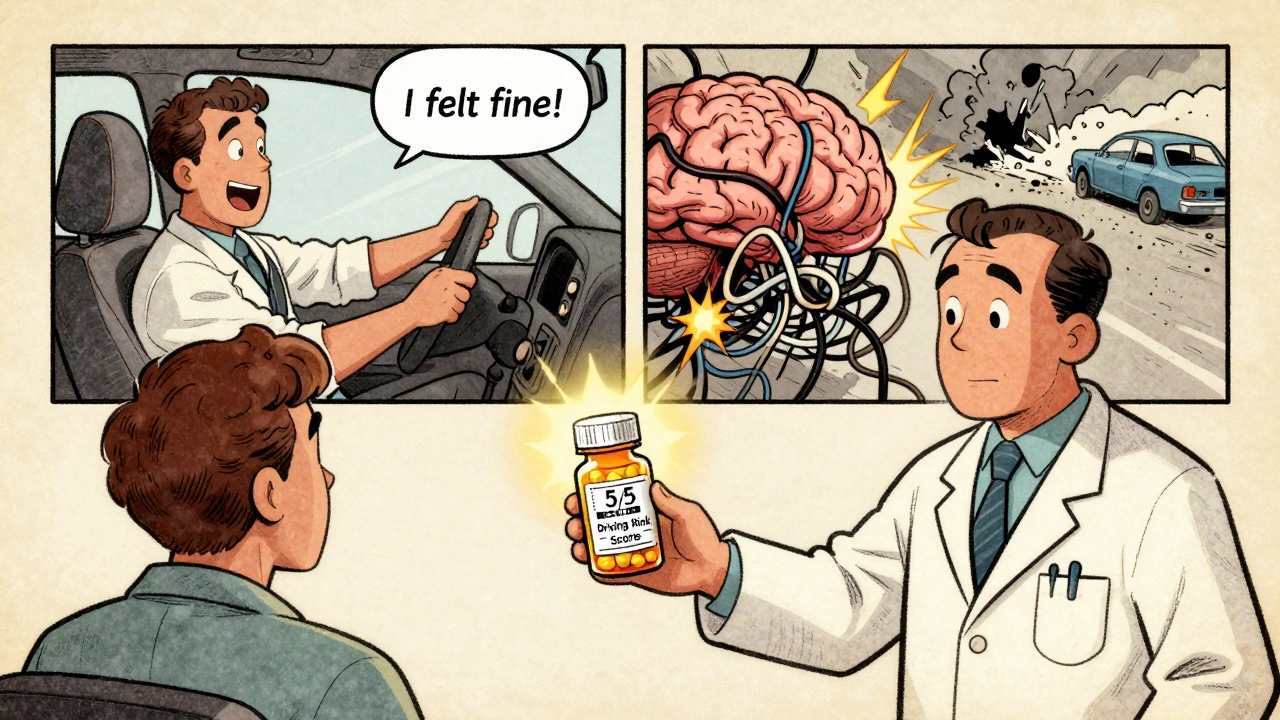
You take your pill like clockwork. Maybe it’s the sleep aid you’ve been using for years, the painkiller for your back, or the allergy medicine you grab off the shelf when your nose won’t stop running. You feel fine. So you get in the car. But here’s the truth: feeling fine doesn’t mean you’re safe to drive. Many common medications slow your reaction time, blur your vision, or make you drowsy without you even realizing it. And in the eyes of the law, that’s just as dangerous as drinking alcohol behind the wheel.
In the U.S., drug-impaired driving causes about 18% of all fatal crashes-second only to alcohol. Yet most people don’t think of their prescription or over-the-counter meds as a danger on the road. That’s a deadly misunderstanding. The problem isn’t just opioids or benzodiazepines. It’s also the cold medicine in your cabinet, the NSAID you take for arthritis, or the antidepressant your doctor prescribed last year. And if you’re over 65, your body processes these drugs differently, making impairment more likely and more severe.
Which Medications Actually Impair Driving?
Not all drugs affect driving the same way. Some hit you fast. Others linger for hours. Here’s what the data shows:
- Benzodiazepines (like diazepam, alprazolam): Used for anxiety and insomnia. These drugs slow brain processing by 25-40%. Studies show they increase crash risk by 40-60%. Combine them with alcohol, and the risk doubles.
- Opioids (oxycodone, fentanyl, codeine): For pain. They cause drowsiness, constricted pupils, and reduce reaction time by up to 300 milliseconds. That’s like adding 10-15 feet to your stopping distance at highway speeds.
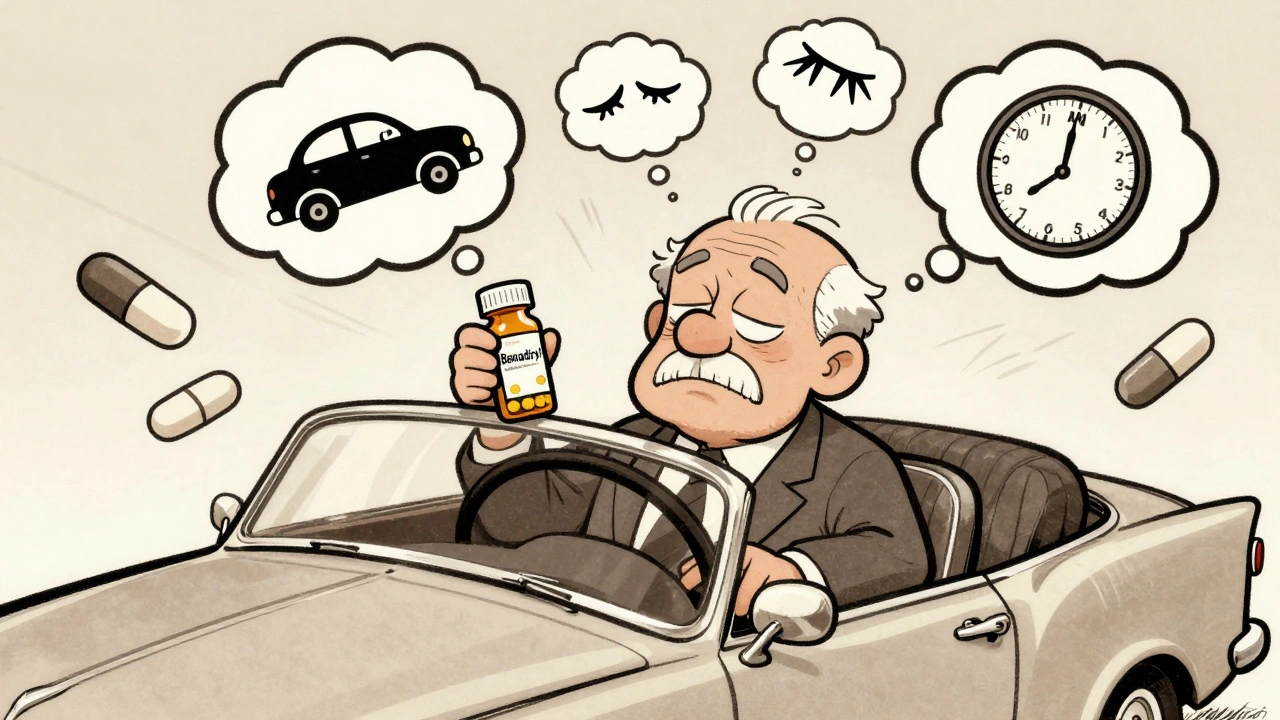
- First-generation antihistamines (diphenhydramine in Benadryl, Tylenol PM): These are in dozens of sleep aids and cold medicines. One dose can impair you as much as a 0.10% blood alcohol level-higher than the legal limit in every U.S. state.
- NSAIDs (ibuprofen, naproxen): Often thought of as harmless. But research shows users have a 58% higher crash risk. Why? They can cause dizziness, blurred vision, and delayed decision-making.
- Tricyclic antidepressants and mirtazapine: These increase motor vehicle accident rates by 40%. The effect isn’t always obvious-you might feel alert but still be slower to react to sudden stops or turns.
- Zolpidem (Ambien): A popular sleep pill. Its effects can last up to 11 hours. Many people take it at night, wake up feeling "normal," and drive to work-only to fail a sobriety test hours later.
Even second-generation antihistamines like loratadine (Claritin) or cetirizine (Zyrtec) aren’t risk-free. They’re safer, yes-but not zero-risk. And if you’re taking more than one medication at a time? That’s where things get dangerous.
Poly-Drug Driving: The Hidden Killer
Most people don’t realize that mixing medications-or mixing meds with alcohol or marijuana-creates a synergy effect. The whole is worse than the sum of its parts.
One study of drivers at trauma centers found that 22% had multiple drugs in their system. One driver might have taken an opioid for pain, a benzodiazepine for anxiety, and a cold pill with diphenhydramine-all in the same day. Individually, each drug might only slightly impair driving. Together? They multiply the effect. Reaction time drops. Judgment crumbles. The brain can’t keep up.
And here’s the scary part: drivers often don’t know they’re impaired. A 2021 AAA survey found that 70% of people who took three or more potentially impairing drugs still drove within two hours of taking them. They felt fine. They weren’t dizzy. They didn’t feel sleepy. But their brain wasn’t working right. That’s the quiet danger of medication impairment-it doesn’t always come with a warning sign.

Legal Consequences Are Real-and Harsh
In most states, you can be charged with DUI for driving under the influence of prescription drugs-even if they were legally prescribed. The law doesn’t care if your doctor told you to take it. If the drug impairs your ability to drive safely, you’re breaking the law.
As of 2025, only 28 states have specific legal limits for prescription drugs in your bloodstream. That means in the other 22, prosecutors don’t need to prove you were over a certain level-they just need to show you were impaired. That’s easier than you think. Police use Drug Recognition Experts (DREs), trained to spot signs like dilated or constricted pupils, poor coordination, slurred speech, and abnormal eye movements. If you’re pulled over and fail a field test, you’re likely facing fines, license suspension, or even jail time.
One Reddit user, u/SafeDriver2023, posted about taking Tylenol PM before bed, waking up at 7 a.m., and driving at 9 a.m. He felt fine. He wasn’t hungover. But the diphenhydramine was still in his system. He failed a field sobriety test. He lost his license for six months. He didn’t know the drug could linger that long.
Why Doctors and Pharmacists Don’t Always Warn You
You’d think your doctor or pharmacist would tell you if your meds could make driving dangerous. But they often don’t.
A 2022 survey found that 68% of patients received no specific driving advice when prescribed a medication with known impairment risks. Only 41% of physicians routinely discuss driving safety during medication consultations. Pharmacists are better-89% now include driving warnings when dispensing-but that still means 11% don’t.
Even the labels on the bottles are vague. "May cause drowsiness" doesn’t tell you how long the effect lasts. It doesn’t say if it’s safe to drive after 4 hours-or 8. The FDA only started requiring "Driving Risk Scores" on labels in May 2023, rating drugs from 1 (minimal risk) to 5 (severe risk). But most existing prescriptions still have outdated labels.
And if you’re over 65? The Beers Criteria-a set of guidelines used by doctors to avoid dangerous drugs in older adults-lists more than 30 medications that should be avoided because of their impact on driving. Yet many older patients are still prescribed them without warning.
What You Can Do to Stay Safe
You don’t have to stop taking your meds. But you need to understand how they affect you.
- Ask your doctor or pharmacist: "Can this medicine make it unsafe for me to drive? How long should I wait after taking it?" Don’t assume it’s fine because you "feel okay."
- Check the label for driving risk scores: Newer prescriptions should have a number from 1 to 5. Avoid driving if it’s 4 or 5.
- Wait longer than you think: For first-gen antihistamines, wait at least 6 hours. For zolpidem, wait 8-12. For opioids, don’t drive for at least 8 hours after the last dose-even if you feel alert.
- Never mix meds with alcohol: Alcohol multiplies the effect of almost every impairing drug.
- Use a self-assessment: Try the University of Iowa’s Driving Simulator Test. It takes 10 minutes. If you can’t complete 15 maneuvers with less than 1.5 lane deviations, you’re not fit to drive.
- Plan ahead: If you’re starting a new medication, take the first dose on a day you don’t need to drive. See how you feel before getting behind the wheel.
The Future Is Here-And It’s Watching You
By 2027, 85% of new cars will have biometric systems that monitor your eyes, steering, and braking patterns to detect impairment. These systems can tell if your eyelids are drooping, if your steering is erratic, or if your reaction time is slowing-without you even knowing it.
Police are also getting better at detection. The NHTSA’s $22 million Prescription Drug Impairment Detection Initiative has developed saliva tests that can identify 12 common prescription drugs with 92.7% accuracy. These tests are being rolled out across 47 states.
But technology won’t fix the root problem: people don’t know they’re at risk. And that’s why awareness matters more than ever.
Bottom Line: Don’t Guess. Test. Ask. Wait.
Driving while impaired by medication isn’t a minor mistake. It’s a leading cause of preventable death. You don’t need to be drunk to be dangerous. You just need to be taking the wrong pill at the wrong time.
If you’re on any medication-prescription or over-the-counter-ask yourself: Could this make me a hazard on the road? If you’re not sure, don’t drive. Wait. Test. Talk to your pharmacist. Your life-and someone else’s-could depend on it.
Can I drive after taking ibuprofen or naproxen?
It depends. For most people, standard doses of ibuprofen or naproxen don’t cause obvious drowsiness. But research shows users have a 58% higher risk of crashing. These drugs can cause dizziness, blurred vision, or delayed reaction time-especially in older adults or if taken with other medications. If you’ve never taken them before, try them on a day you’re not driving. If you feel off at all, don’t get behind the wheel.
Is it illegal to drive while taking prescribed medication?
Yes. It doesn’t matter if your doctor prescribed it. If the drug impairs your ability to drive safely, you can be charged with DUI. In most states, you don’t need to be over a legal limit-you just need to be impaired. Police use field sobriety tests and Drug Recognition Experts to determine this. Even a legally prescribed opioid or benzodiazepine can lead to arrest, fines, or license suspension.
How long after taking Benadryl is it safe to drive?
The FDA recommends waiting at least 4-6 hours after taking diphenhydramine (Benadryl). But studies show impairment can last up to 8-10 hours, especially in older adults or those taking other meds. One dose can impair you as much as a 0.10% blood alcohol level-higher than the legal limit in every U.S. state. If you took it at night for sleep, don’t assume you’re safe by morning. Wait until you’re 100% sure your reflexes and focus are back to normal.
Do older adults face higher risks from medication-related driving impairment?
Yes. As we age, our bodies process drugs more slowly. The liver and kidneys don’t remove medication as efficiently, and brain sensitivity increases. A dose that’s safe for a 40-year-old can be dangerously impairing for a 70-year-old. The Beers Criteria specifically lists over 30 medications that should be avoided in adults over 65 because of their impact on driving. If you’re over 65 and on any new medication, ask your doctor if it’s on that list.
What should I do if I’m taking multiple medications?
Ask your pharmacist to review all your meds-including supplements and OTC drugs-for potential interactions. Taking three or more impairing drugs dramatically increases crash risk. Even if each drug alone is low-risk, together they can create a synergistic effect that’s far more dangerous. Use the Driving Risk Score on new labels (1-5) to identify high-risk drugs. If you’re on a 4 or 5, avoid driving entirely until you’ve talked to your doctor about alternatives.
Are there tools to test if I’m fit to drive after taking medication?
Yes. The University of Iowa developed a free 10-minute Driving Simulator Test that assesses your reaction time, lane control, and braking response. If you make more than 1.5 lane deviations during the test, you’re not safe to drive. Many pharmacies and senior centers now offer access to this tool. It’s not perfect-but it’s far better than guessing whether you’re "fine."

Jack Dao
December 3, 2025 AT 17:16Lynn Steiner
December 4, 2025 AT 09:32Elizabeth Grace
December 4, 2025 AT 23:27Roger Leiton
December 6, 2025 AT 16:10Ella van Rij
December 7, 2025 AT 20:58dave nevogt
December 8, 2025 AT 12:02Paul Keller
December 10, 2025 AT 02:45Steve Enck
December 10, 2025 AT 11:55Steve World Shopping
December 10, 2025 AT 16:01Rebecca M.
December 11, 2025 AT 17:41Joel Deang
December 12, 2025 AT 17:39