When women start experiencing hot flashes, night sweats, or mood swings during menopause, hormone therapy can be a game-changer. But it’s not as simple as just picking up a pill. The right hormone therapy combination depends on your body, your history, and even how you prefer to take it. Many women assume all HRT is the same, but the differences between oral tablets, patches, gels, and IUDs can mean the difference between relief and risk.
Why Combination Therapy Matters
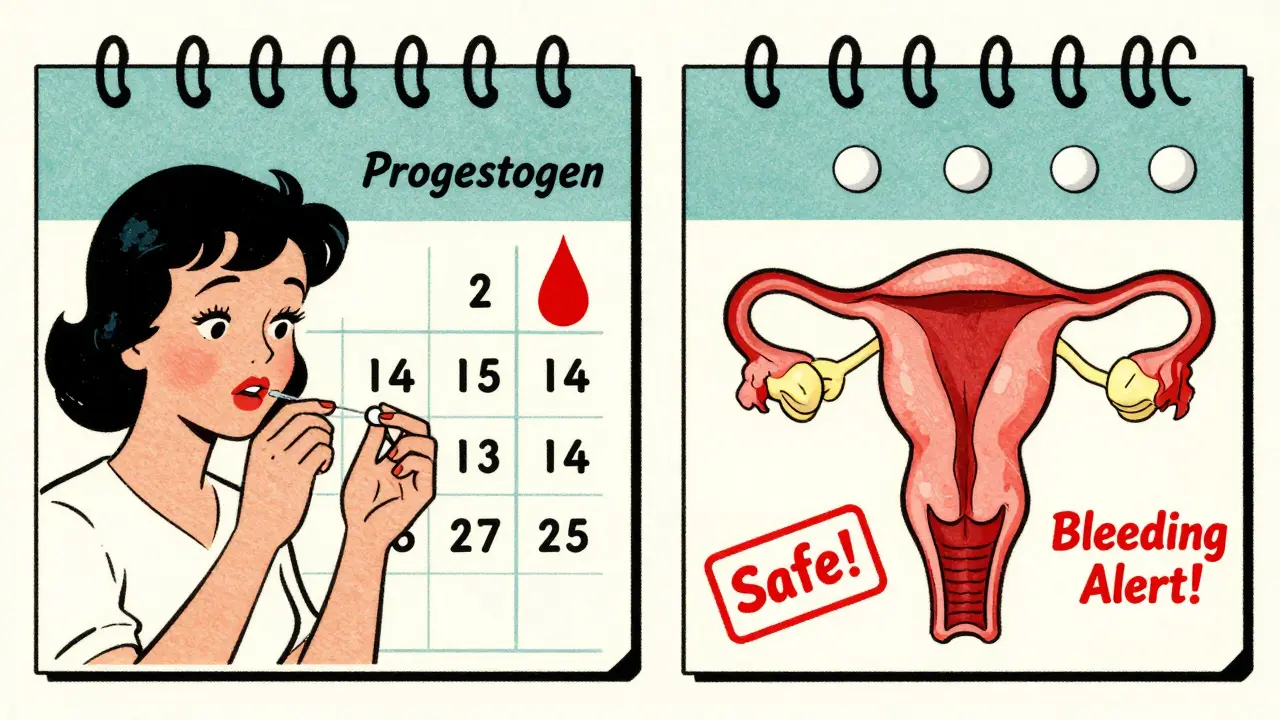
If you still have your uterus, taking estrogen alone isn’t safe. Estrogen causes the lining of your uterus to thicken. Left unchecked, that can lead to endometrial hyperplasia - and eventually, cancer. That’s why women with a uterus need a combination of estrogen and progestogen. Progestogen keeps the uterine lining thin, preventing dangerous growth. For women who’ve had a hysterectomy, estrogen-only therapy is the standard. It’s simpler, safer for the uterus, and often better tolerated. But if you still have your uterus, the type of combination you use depends on whether you’re still having periods or not.Sequential vs. Continuous: Two Different Approaches
There are two main types of combination therapy, and choosing the wrong one can lead to unwanted bleeding or ineffective symptom control. Sequential combined HRT is for women who are still having periods - whether regular or irregular. You take estrogen every day, then add progestogen for the last 10 to 14 days of the month. This mimics your natural cycle. You’ll likely get a withdrawal bleed each month, which is normal and expected. This method is often used during perimenopause when cycles are still changing. Continuous combined HRT is for women who haven’t had a period for a full year. You take both estrogen and progestogen every single day, with no breaks. There’s no monthly bleed - and that’s the point. It’s designed for postmenopausal women who no longer need a menstrual pattern. Studies show this approach may lower the risk of colon cancer by 18% and type 2 diabetes by 21%, based on data from the Women’s Health Initiative. Switching between these without medical guidance can cause confusion. If you start continuous therapy too early - while still having periods - you’ll likely get breakthrough bleeding. If you stick with sequential therapy too long after menopause, you might get unnecessary monthly bleeds with no added benefit.Generic Options: What’s Actually in Your Pills
Most hormone therapy prescriptions today are generic. They’re cheaper, just as effective, and widely available. Here’s what you’re likely to get:- Conjugated estrogens - 0.3mg, 0.45mg, or 0.625mg tablets. These are derived from horse urine and have been used for decades.
- Estradiol - 0.5mg or 1mg tablets. This is the same estrogen your body naturally makes. Many doctors now prefer it because it’s more bioidentical.
- Medroxyprogesterone acetate - 2.5mg, 5mg, or 10mg tablets. A synthetic progestin, commonly used in generic combinations.
- Micronized progesterone - 100mg or 200mg capsules. This is natural progesterone, derived from plants. It’s more expensive but has a better safety profile for breast cancer risk.
Delivery Methods: Patches, Gels, and IUDs - Which Is Right?
How you take your hormones matters just as much as what you take. Oral pills aren’t the only option - and they’re not always the safest. Oral tablets go through your liver first. That increases your risk of blood clots by 2 to 3 times compared to other methods. The absolute risk is still low - about 1 in 1,000 women per year - but it adds up if you’re over 60 or have other risk factors like obesity or a history of clots. Transdermal patches, gels, and sprays deliver hormones through your skin. They bypass the liver, so they don’t raise clotting risk the same way. Studies show transdermal estrogen has a similar risk profile to not taking HRT at all. That’s why experts now recommend them as the first choice for women over 50, especially those with high blood pressure, migraines, or a history of clots. The Mirena IUD is a game-changer for women who need progestogen. It releases a low dose of levonorgestrel directly into the uterus, protecting the lining without flooding your whole body with hormones. Many women use it with a low-dose estrogen patch or gel. This combo reduces bleeding and minimizes systemic side effects like breast tenderness or mood swings.Who Should Avoid HRT - And Who Benefits Most
Not everyone is a candidate. The biggest red flags include:- History of blood clots, stroke, or heart attack
- Unexplained vaginal bleeding
- History of estrogen-sensitive breast cancer
- Active liver disease
Common Challenges and How to Handle Them
Many women stop HRT because of side effects - but most of these are temporary. Breakthrough bleeding is the #1 reason women quit. Up to 20% experience spotting in the first 3 to 6 months. It usually settles down. If it doesn’t, your dose or delivery method may need adjusting. Don’t assume it’s cancer - get it checked, but don’t panic. Breast tenderness often fades after a few weeks. Switching from oral to transdermal estrogen can help. Mood changes are less common than people think. If you’re feeling unusually down or anxious, it might be the progestogen. Try switching from medroxyprogesterone to micronized progesterone - many women report better mood stability. Application issues are real. Patches can fall off if you sweat too much. Gels need 60 minutes to dry before you hug someone - or you risk transferring hormones to your partner. Read the instructions. Ask your pharmacist to demonstrate.


Joy Nickles
December 31, 2025 AT 18:08Emma Hooper
January 2, 2026 AT 13:46Martin Viau
January 4, 2026 AT 00:20Robb Rice
January 4, 2026 AT 03:46Retha Dungga
January 5, 2026 AT 19:50Aaron Bales
January 6, 2026 AT 21:53Urvi Patel
January 7, 2026 AT 16:27anggit marga
January 9, 2026 AT 09:02Marilyn Ferrera
January 9, 2026 AT 09:03Harriet Hollingsworth
January 9, 2026 AT 16:49Deepika D
January 11, 2026 AT 07:37Bennett Ryynanen
January 11, 2026 AT 07:47Chandreson Chandreas
January 12, 2026 AT 16:47